Appendices
Supportive care in cancer refers to the following five domains:
- physical domain, which includes a wide range of physical symptoms that may be acute, relatively short-lived or ongoing, requiring continuing interventions or rehabilitation (NBCC & NCCI 2003)
- psychological domain, which includes a range of issues related to the person’s mental health and personal relationships (NBCC & NCCI 2003)
- social domain, which includes a range of social and practical issues that will impact on the individual and family such as the need for emotional support, maintaining social networks and financial concerns (NICE 2004)
- information domain, which includes access to information about cancer and its treatment, support services and the health system overall (NBCC & NCCI 2003)
- spiritual domain, which focuses on the person’s changing sense of self and challenges to their underlying beliefs and existential concerns (NICE 2004).
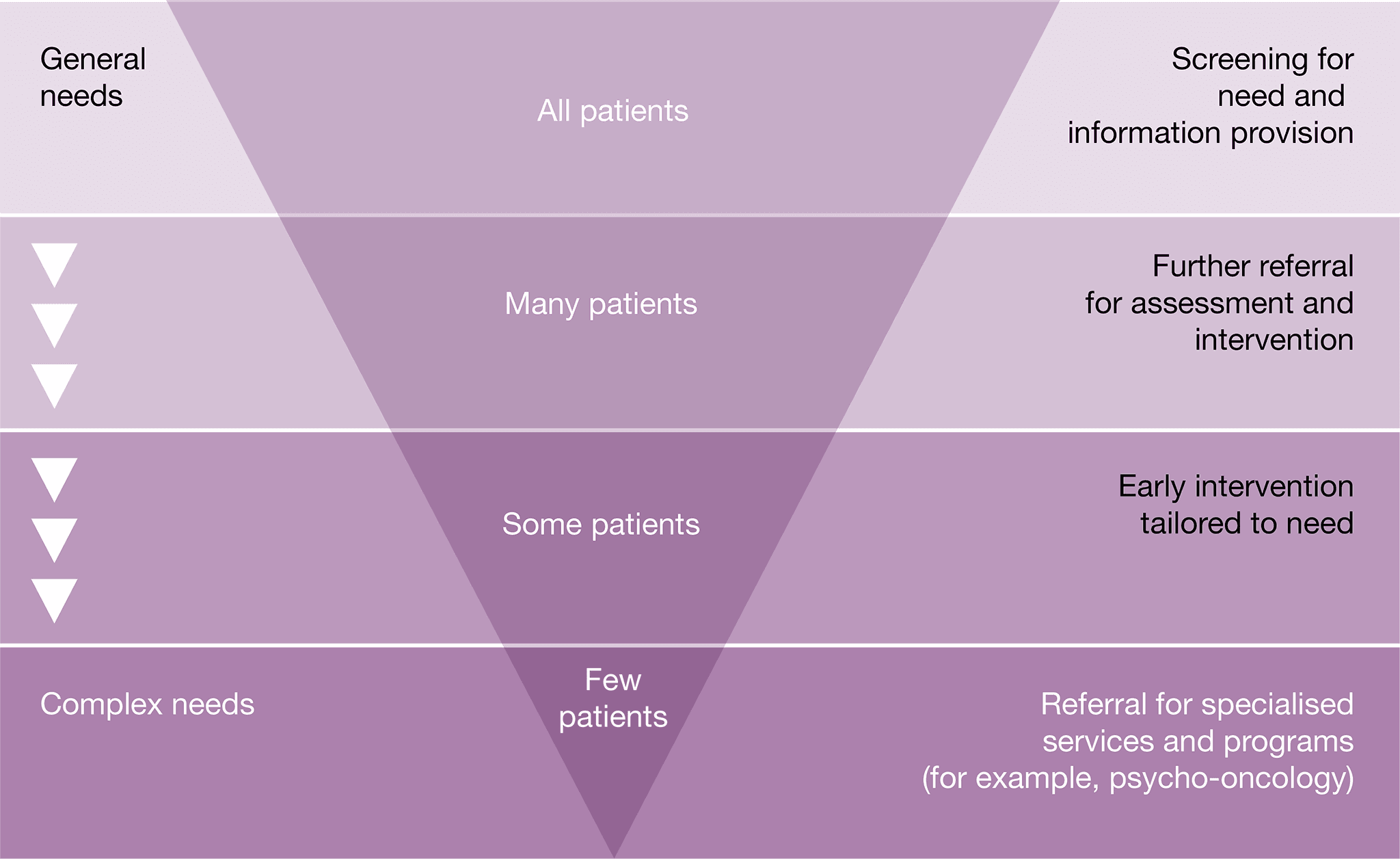
Fitch’s (2000) model of supportive care recognises the variety and level of intervention required at each critical point as well as the need to be specific to the individual. The model targets the type and level of intervention required to meet patients’ supportive care needs.
Some patients with CUP will require specialised intervention. Common indicators in patients with CUP that may require referral to appropriate health professionals and/or organisations include the following.
Physical needs
- Patients should receive treatment for physical symptoms.
- Breathlessness and coughing often create anxiety. Consider strategies such as exploring the meaning of breathlessness, breathing retention exercises, teaching relaxation and distraction techniques, and encouraging planning and pacing (NBCC & NCCI 2003). Referral to physiotherapy, occupational therapy or pulmonary rehabilitation may be required.
- If oxygen is medically indicated, this can be arranged through the relevant state aids and equipment program.
- Alteration of cognitive functioning in patients treated with chemotherapy and radiation therapy requires strategies such as maintaining written notes or a diary and repetition of information (NBCC & NCCI 2003).
- Patients with weight loss or bony metastasis often experience pain sitting or lying. Appropriate devices should be considered to improve overall comfort and engagement in activities.
- Physical decline is common in patients with CUP. Maintenance of function should be encouraged. Referral to a physiotherapist should be considered if further advice is required.
- Should a patient’s physical function deteriorate, referral to occupational therapy for review of their home environment should be considered if compensation strategies are required.
- Referral to a pharmacist may be useful for people managing multiple medications.
- Decline in mobility and/or functional status as a result of treatment should be monitored.
- Malnutrition can occur as a result of disease or treatment. Validated malnutrition screening tools should be used at the key points in the care pathway to identify patients at risk of malnutrition and refer to a dietitian for nutrition intervention.
- Fatigue/change in functional capacity is a common symptom, and patients may benefit from referral to occupational therapy.
- Focal deficits may affect the patient’s mobility and ability to take part in everyday activities. Referral to an occupational therapist and a physiotherapist for assessment, education, intervention and compensatory strategies may assist with maintaining mobility.
- Dysphasia may occur, and referral to a speech pathologist may be needed (Taillibert et al. 2004).
Psychological needs
- Many patients with CUP find the uncertainty surrounding their disease and the inability to treat it difficult and would welcome the opportunity to ask questions and learn about others’ experiences (Boyland & Davis 2008).
- Many patients with CUP and their clinicians have a poor understanding of their illness, have difficulty in explaining their illness to others, and have a sense of frustration in health professionals not having the answers (Boyland & Davis 2008, Karapetis et al. 2016).
- It is important to ensure the patient understands that they are being investigated for a possible cancer diagnosis, even prior to a tissue diagnosis being obtained.
- Patients with CUP will most likely undergo extensive testing, and support and information should be provided to assist with any distress while undergoing these tests (Wagland et al. 2017).
- The GP should inform the patient that they might have cancer early on in the diagnostic investigation process. Good communication from experts at this stage is very important.
- Depressive symptoms are higher in people with CUP when compared with people with cancer of a known origin, so they require more psychosocial support and specific interventions (Hyphantis et al. 2013).
- Palliative care can improve physical symptom control and quality of life for people with cancer including improving the capacity of patients to come to terms with diagnostic and prognostic uncertainty (Temel et al. 2017).
- GPs play an important role in coordinating care for patients, including assisting with side effects and offering support when questions or worries arise. For most patients, simultaneous care provided by their GP is very important (Lang et al. 2017).
- For some populations (culturally and linguistically diverse backgrounds, Aboriginal and Torres Strait Islanders, and lesbian, gay, bisexual, transgender and intersex (LGBTI) communities) a cancer diagnosis can come with additional psycho-social complexities. Access to expert health
- professionals with knowledge specific to the psychosocial needs of these groups may be required.
- Patients with CUP should be regularly screened for depression and anxiety as a result of increased dependency. If loss of independence is a factor contributing to depression, then referral to physiotherapy and occupational therapy may restore some independence and assist some people. Referral to a psychologist or psychiatrist may also be helpful in managing the depression.
- Some people may have disabling symptoms and may benefit from referral to a psychology service.
- Distress and depression can be just as common in carers and family members, including children.
- Cognitive changes as a result of treatment (such as altered memory, attention and concentration) may require assessment.
- Help with the emotional distress of dealing with a cancer diagnosis, stress and adjustment difficulties may be required (Hyphantis et al. 2015).
- Difficulty with social interactions can place the patient at higher risk of depression. A referral to a speech pathologist to manage and maximise any communication impairments, and an occupational therapist or psychologist for social skills training, may help to reduce psychosocial difficulties.
- Patients may need support with body image concerns, fatigue, existential anxiety, treatment phobias, anxiety/depression, interpersonal problems, returning to work, and sexuality concerns.
- Consider a referral to a psychologist, psychiatrist or social worker if the patient is:
- displaying emotional cues such as tearfulness, distress, avoidance and withdrawal
- preoccupied with or dwelling on thoughts about cancer and death
- displaying fears about the treatment process and/or the changed goals of their treatment
- worried about loss associated with their daily function, dependence on others and loss of dignity
- becoming isolated from family and friends and withdrawing from people and activities that they previously enjoyed
- feeling hopeless and helpless about the impact that brain cancer is having on their life and the disruption to their life plans
- struggling with communicating to family and loved ones about the implications of their cancer diagnosis and treatment
- experiencing changes in sexual intimacy, libido and function
- struggling with the diagnosis of metastatic or advanced disease
- having difficulties transitioning to palliative care.
Social/practical needs
- A diagnosis of CUP can have significant financial, social and practical impacts on patients, carers and families.
- The additional costs related to management are significant. A referral to a social worker should be considered for further assessment and identification of financial and practical support available.
- Significant restrictions to social activities may require referral to a social worker, occupational therapist, psychologist or psychiatrist.
- Patients may need advice about safe driving.
- Consider the need for appropriate information for people from culturally and linguistically diverse backgrounds.
Information needs
- Patients with CUP will most likely undergo extensive testing, and support and information should be provided to assist with any distress while undergoing these tests (Wagland et al. 2017).
- CUP patients are more likely to want written information about their type of cancer and tests received but less likely to understand explanations of their condition (Wagland et al. 2017).
- Ensure the patient understands that they have been diagnosed with CUP, and that they understand the ramifications of this diagnosis.
- Assist the patient in explaining their diagnosis to their family. Audio recordings may be a helpful resource for patients (Pitkethly et al. 2008).
- Offer individualised cancer information that meets the needs of the patient and carer (this may involve advice from health professionals as well as written and visual resources).
- Offer advice on how to access information from websites, community sources and national cancer services. A list of websites has been included under Resource List.
Spiritual needs
- Multidisciplinary teams should have access to suitably qualified, authorised and appointed spiritual caregivers who can act as a resource for patients, carers and staff. They should also have up-to date awareness of local community resources for spiritual care.
- Patients with cancer and their families should have access to spiritual support appropriate to their needs throughout the cancer journey.







