Pancreatic cancer
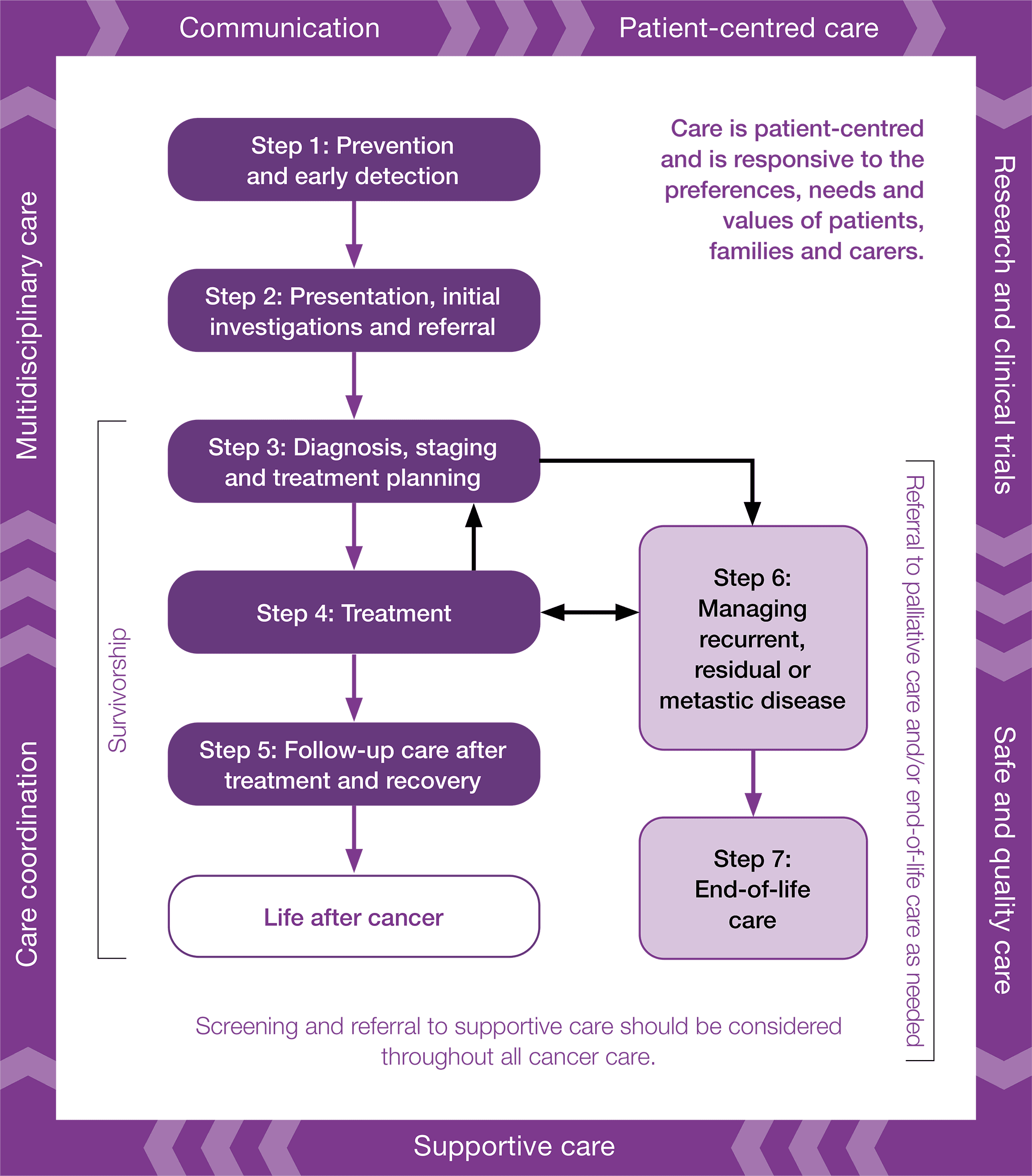
Optimal care pathways map seven key steps in cancer care. Each of these steps outlines nationally agreed best practice for the best level of care. While the seven steps appear in a linear model, in practice, patient care does not always occur in this way but depends on the particular situation (e.g. the type of cancer, when and how the cancer is diagnosed, prognosis, management, the patient’s decisions and their physiological response to treatment).
The principles underpinning optimal care pathways always put patients at the centre of care throughout their experience and prompt the healthcare system to deliver coordinated care.
The optimal care pathways do not constitute medical advice or replace clinical judgement, and they refer to clinical guidelines and other resources where appropriate.
Evidence-based guidelines, where they exist, should inform timeframes. Treatment teams need to recognise that shorter timeframes for appropriate consultations and treatment can promote a better experience for patients. Three steps in the pathway specify timeframes for care. They are designed to help patients understand the timeframes in which they can expect to be assessed and treated, and to help health services plan care delivery in accordance with expert-informed time parameters to meet the expectation of patients. These timeframes are based on expert advice from the Pancreatic Cancer Working Group.
Timeframes for care
|
Step in pathway |
Care point |
Timeframe |
|
Presentation, initial investigations and referral |
Signs and symptoms |
Presenting symptoms should be promptly and clinically triaged with a health professional |
|
Initial investigations initiated by GP |
Patients who present with jaundice should be referred for tests within 48 hours and followed up rapidly Other symptoms require review within 2 weeks |
|
|
Referral to specialist |
Patients with suspected or proven pancreatic cancer should be seen by a specialist within 1 week of referral to the specialist |
|
|
Diagnosis, staging and treatment planning |
Diagnosis and staging |
Diagnostic and staging investigations should be completed within 2 weeks of referral |
|
Multidisciplinary meeting and treatment planning |
The patient case must be discussed within 1 week of completion of the diagnostic and staging investigations and a management plan finalised |
|
|
Treatment |
Surgery |
Surgery should be undertaken within 4 weeks of initial diagnosis, depending on urgency and modality |
|
Systemic chemotherapy and/or radiation therapy |
Treatment should begin within 4 weeks of initial diagnosis, depending on urgency and modality Adjuvant chemotherapy in the postoperative setting should begin within 12 weeks of surgery |
Seven steps of the optimal care pathway
Step 1: Prevention and early detection
Step 2: Presentation, initial investigations and referral
Step 3: Diagnosis, staging and treatment planning
Step 4: Treatment
Step 5: Care after initial treatment and recovery
Step 6: Managing recurrent, residual or metastatic disease
Step 7: End-of-life care
In Australia the incidence of pancreatic cancer has remained stable over the past three decades, with 10 cases per 100,000 people in 1982 and 12 cases per 100,000 people in 2016 (Cancer Australia 2020b). The average age at diagnosis is 72.8 years (AIHW 2017a). Pancreatic cancer has a very poor prognosis, and five-year survival rates are extremely low. Median survival from diagnosis ranges from 10 to 30 months (Lambert el al. 2019). In Australia over the past three decades the five-year survival rate has increased slightly from 3.2 per cent between 1987 and 1991 to 11 per cent between 2012 and 2016 (Cancer Australia 2020b). Despite the increase in survival, pancreatic cancer still has the lowest survival rate of all cancer types, with mortality-to-incidence ratio approaching 1 (0.83; Cancer Australia 2019b). Even if there are good initial treatment outcomes, the recurrence rate is very high. Given the poor prognosis of this cancer at present, for most patients, treatment is often given with palliative, rather than curative, intent. Early specialist palliative care will be required for patients with pancreatic cancer.
This optimal care pathway covers pancreatic adenocarcinoma. Pancreatic neuroendocrine tumours (PNETs) are not included in this pathway, given the differences in the risk factors and management of these tumours.
This step outlines recommendations for the prevention and early detection of pancreatic cancer.
Evidence shows that not smoking, avoiding or limiting alcohol intake, eating a healthy diet, maintaining a healthy body weight, being physically active, being sun smart and avoiding exposure to oncoviruses or carcinogens may help reduce cancer risk (Cancer Council Australia 2018).
Although the aetiology of pancreatic cancer is unknown, the current prevention strategies involve reducing risk factors. The two most effective prevention strategies include avoiding tobacco smoking and maintaining a normal body weight (American Cancer Society 2019; Xu et al. 2018). Some studies suggest a change in diet may decrease the risk of pancreatic cancer by decreasing soft drink and sugar consumption and increasing consumption of whole grains and vegetables (Lei et al. 2016; Pericleous et al. 2014).
The risk factors for developing pancreatic cancer include:
- tobacco smoking (most established risk factor; risk increases significantly with greater intensity and duration) (Arriaga et al. 2019)
- cystic lesions of the pancreas
- obesity
- increased consumption of red meat and processed meat
- a family history of pancreatic cancer
- older age
- chronic pancreatitis
- longstanding type 2 diabetes mellitus
- male gender
- Asian or Pacific Islander ethnicity
- chronic alcohol consumption
- liver cirrhosis
- stomach infections with the bacterium Helicobacter pylori, which causes stomach ulcers
- heavy occupational exposure to certain pesticides, dyes and chemicals used in metal refining (Cancer Australia 2017a).
Having certain hereditary conditions also increase a person’s risk of pancreatic cancer:
- hereditary pancreatitis syndrome
- hereditary nonpolyposis colon cancer (HNPCC – Lynch syndrome)
- Peutz-Jeghers syndrome
- hereditary BRACA2-related breast and ovarian cancer syndrome
- familial atypical multiple mole melanoma (FAMMM) syndrome
- ataxia-telangiectasia syndrome (ATM mutation)
- Li-Fraumeni syndrome (TP53 mutation).
There is no recommended population screening program for pancreatic cancer in Australia.
The cancer antigen 19-9 (CA 19-9) tumour marker is not recommended as a population screening tool for pancreatic cancer due to the low sensitivity and specificity of the test, but rather it should be used as a marker of response to treatment (NCI 2019a).
For people with a strong family history of pancreatic cancer (those who have two or more close relatives affected by pancreatic cancer) and those with a family history of pancreatic cancer–related hereditary conditions (BRCA 2, Lynch syndrome, FAMMM syndrome and Peutz-Jeghers syndrome), it is recommended that they are referred to a familial cancer service, geneticist or oncologist for genetic testing (Goggins et al. 2019).
Potential imaging for monitoring pancreatic cancer in high-risk populations includes a range of imaging modalities; however, endoscopic ultrasound is generally accepted as the most sensitive imaging test for small pancreatic head tumours. Blood samples (CA 19-9, carcinoembryonic antigen [CEA] and liver biochemistry) are also collected.
This step outlines the process for the general practitioner to initiate the right investigations and refer to the appropriate specialist in a timely manner. The types of investigations the general practitioner undertakes will depend on many factors, including access to diagnostic tests, the availability of medical specialists and patient preferences.
Many cases present with non-specific symptoms or are asymptomatic until advanced stages of the disease. The following signs and symptoms should be investigated:
- acute pancreatitis where the cause is not alcohol ingestion and gallstones are not evident
- new-onset diabetes
- jaundice that is progressive, together with unexplained weight loss and abdominal pain that may radiate to the back (the jaundice may also be accompanied with dark urine, light-coloured stools and itchy skin)
- pain, which is often severe, unrelenting and of a short duration
- unexplained weight loss
- pale and greasy stools
- nausea and vomiting
- constipation
- fatigue
- enlargement of gall bladder
- blood clot in the leg without a clear risk factor
- incidental lesions found on radiology (Freelove & Walling 2006; Kamisawa et al. 2016).
The presence of multiple signs and symptoms, particularly in combination with other underlying risk factors, indicates an increased risk of pancreatic cancer.
Increasingly, incidental diagnosis may occur with pancreatic abnormalities detected on investigation for other complaints.
The incidence of pancreatic cancer in people below 40 years is extremely low. The cause of jaundice in people aged under 40 years is more likely to be caused by other conditions such as alcoholism or hepatitis. People aged under 40 years with jaundice should be referred to non–cancer related pathways.
Presenting symptoms should be promptly and clinically triaged with a health professional.
Depending on the presenting symptoms and risk factors, the general practitioner examinations include the following.
Where there is suspicion of pancreatic cancer, consider:
- an abdominal CT scan with pancreatic protocol
- serum CA 19-9 and liver function tests
- early referral (strongly indicated), usually prior to a definitive diagnosis being made.
Where jaundice is present, the following should be performed urgently:
- liver function tests
- abdominal ultrasound
- CT where appropriate.
An abnormal result should be discussed face to face with the patient and information provided.
Patients who present with jaundice should be referred for tests within 48 hours and followed up rapidly.
Other symptoms require review within two weeks (NICE 2015).
If the cancer diagnosis is confirmed or the results are inconsistent or indeterminate, the general practitioner must refer the patient to an appropriate specialist (gastroenterologist, oncologist or hepatopancreaticobiliary [HPB] surgeon with professional expertise in pancreatic cancer management and access to a multidisciplinary team) to make the diagnosis. In patients with locally advanced, non-metastatic disease, if resectability needs to be determined, referral should be to an HPB surgeon.
Patients should be enabled to make informed decisions about their choice of specialist and health service. General practitioners should make referrals in consultation with the patient after considering the clinical care needed, cost implications (see referral options and informed financial consent), waiting periods, location and facilities, including discussing the patient’s preference for health care through the public or the private system.
Referral for suspected or diagnosed pancreatic cancer should include the following essential information to accurately triage and categorise the level of clinical urgency:
- important psychosocial history and relevant medical history
- family history, current symptoms, medications and allergies
- results of current clinical investigations (imaging and pathology reports)
- results of all prior relevant investigations
- notification if an interpreter service is required.
Many services will reject incomplete referrals, so it is important that referrals comply with all relevant health service criteria.
If access is via online referral, a lack of a hard copy should not delay referral.
The specialist should provide timely communication to the general practitioner about the consultation and should notify the general practitioner if the patient does not attend appointments.
Aboriginal and Torres Strait Islander patients will need a culturally appropriate referral. To view the optimal care pathway for Aboriginal and Torres Strait Islander people and the corresponding quick reference guide, visit the Cancer Australia website. Download the consumer resources – Checking for cancer and Cancer from the Cancer Australia website.
All patients with suspected or proven pancreatic cancer should be seen by a specialist (gastroenterologist, oncologist or HPB surgeon) with expertise in pancreatic cancer management and linked to a multidisciplinary team within one week of referral to the specialist.
The patient’s general practitioner should consider an individualised supportive care assessment where appropriate to identify the needs of an individual, their carer and family. Refer to appropriate support services as required. See validated screening tools mentioned in Principle 4 ‘Supportive care’.
A number of specific needs may arise for patients at this time:
- assistance for dealing with the emotional distress and/or anger of dealing with a potential cancer diagnosis, anxiety/depression, interpersonal problems and adjustment difficulties
- management of physical symptoms including chronic pain and fatigue
- encouragement and support to increase levels of exercise (Cormie et al. 2018; Hayes et al. 2019).
For more information refer to the National Institute for Health and Care Excellence 2015 guidelines, Suspected cancer: recognition and referral.
For additional information on supportive care and needs that may arise for different population groups, see Appendices A and B, and special population groups.
The general practitioner is responsible for:
- providing patients with information that clearly describes to whom they are being referred, the reason for referral and the expected timeframes for appointments
- requesting that patients notify them if the specialist has not been in contact within the expected timeframe
- considering referral options for patients living rurally or remotely
supporting the patient while waiting for the specialist appointment (Cancer Council nurses are available to act as a point of information and reassurance during the anxious period of awaiting further diagnostic information; patients can contact 13 11 20 nationally to speak to a cancer nurse).
Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
Step 3 outlines the process for confirming the diagnosis and stage of cancer and for planning subsequent treatment. The guiding principle is that interaction between appropriate multidisciplinary team members should determine the treatment plan.
The treatment team, after taking a thorough medical history and making a thorough medical examination of the patient, should undertake the following investigations under the guidance of a specialist.
Most diagnostic procedures should be completed prior to the MDM. Diagnosis of a mass is primarily by imaging. Biopsy is only required where there is diagnostic uncertainty, or where tissue is required for further management or clinical trials. Contrary to the situation with most cancers, definitive tissue diagnosis prior to the multidisciplinary planning is not recommended.
The following investigation is suggested (to be completed first if not already performed):
- contrast-enhanced CT scan.
If diagnostic uncertainty remains, the following investigations are recommended:
- endoscopic ultrasound with or without biopsy
- contrast-enhanced MRI of the pancreas or magnetic resonance cholangiopancreatography (MRCP) in patients who cannot tolerate contrast or where diagnostic uncertainty remains (Pietryga & Morgan 2015)
- diagnostic laparoscopy with or without laparoscopic ultrasound when resection is planned
Diagnostic and staging (see section 3.2) investigations should be completed within two weeks of referral.
Between five and 10 per cent of pancreatic cancers arise due to a genetic predisposition. A referral to a familial cancer service should be considered for all patients newly diagnosed with pancreatic cancer, particularly if any of the following features are noted:
- a family history of pancreatic cancer
- young age of diagnosis (< 60 years)
- a personal and/or family history of melanoma, breast, ovarian, stomach or colorectal cancer
- a family history of chronic pancreatitis
- Ashkenazi Jewish ancestry.
Genetic testing is sometimes able to identify the cause of pancreatic cancer in an affected individual and, if relevant, their family. An assessment at a familial cancer service can determine if genetic testing is appropriate. Genetic testing can involve testing a single gene or multiple genes at the same time. Where possible, genetic testing will begin in a person affected by pancreatic cancer to identify a predisposing heritable gene mutation. Identifying a gene mutation could improve access to targeted treatment (such as the use of PARP inhibitor therapy in a BRCA gene mutation carrier with advanced pancreatic cancer) and ensure that any other associated cancer risk can also be managed. If a gene mutation is identified, predictive testing will also be available to relatives to see if they have inherited the gene mutation or not. Genetic counselling and fully informed consent is required before proceeding with genetic testing.
If an affected individual or family does not meet the criteria for funded genetic testing, the option of self-funded genetic testing may be discussed. Self-funded genetic testing is increasingly becoming an option as the cost of genetic testing continues to reduce and due to the potential therapeutic implications if a relevant gene mutation is identified.
If an affected individual is unsure or unable to proceed with genetic counselling and/or testing, the option of DNA storage should be discussed as soon as possible. DNA storage may allow their family members to access genetic testing in the future even if the affected individual is unable to or chooses not to proceed with genetic testing.
Visit the Centre for Genetics Education website for basic information about cancer in a family.
Pharmacogenetics describes how individual genetic differences can lead to differences in the way certain medicines interact with the body. These interactions can affect the effectiveness of medications and any side effects. Applying pharmacogenetics to treatment planning may help patients to be prescribed the most appropriate treatment at the optimal dose from the beginning of treatment (NHMRC 2013).
Staging is a critical element in treatment planning and should be clearly documented in the patient’s medical record. Synoptic reporting is encouraged where operative resection has occurred and pathological staging is available. The most widely used staging tools for pancreatic cancer are the American Joint Committee on Cancer’s TNM staging system and stage grouping. The imaging modalities used for diagnosis also allow for simultaneous staging of pancreatic cancer. The pancreatic cancer can be diagnosed and staged as resectable or borderline resectable, locally advanced or metastatic.
Staging for pancreatic cancer involves these tests:
- CT chest/abdominal/pelvis and positron emission tomography (PET)
- MRI pancreatic and/or liver
- laparoscopy plus or minus laparoscopic ultrasound for high-risk patients.
Visit the Cancer Institute New South Wales website for information about understanding the stages of cancer.
Patient performance status is a central factor in cancer care and should be clearly documented in the patient’s medical record.
Performance status should be measured and recorded using an established scale such as the Karnofsky scale or the Eastern Cooperative Oncology Group (ECOG) scale.
A number of factors should be considered at this stage:
- the patient’s overall condition, life expectancy, personal preferences and decision- making capacity
- discussing the multidisciplinary team approach to care with the patient
- appropriate and timely referral to an MDM
- pregnancy and fertility
- support with travel and accommodation
- teleconferencing or videoconferencing as required
The multidisciplinary team should meet to discuss newly diagnosed patients before definitive treatment so that a treatment plan can be recommended and there can be early preparation for the post-treatment phase. The patient case must be discussed within one week of completing the diagnostic and staging investigations and a management plan should be finalised. The level of discussion may vary, depending on the patient’s clinical and supportive care factors. Some patients with non-complex cancers may not be discussed by a multidisciplinary team; instead the team may have treatment plan protocols that will be applied if the patient’s case (cancer) meets the criteria. If patients are not discussed at an MDM, they should at least be named on the agenda for noting. The proposed treatment must be recorded in the patient’s medical record and should be recorded in an MDM database where one exists.
Teams may agree on standard treatment protocols for non-complex care, facilitating patient review (by exception) and associated data capture.
Results of relevant tests and access to images should be available for the MDM. Information about the patient’s concerns, preferences and social and cultural circumstances should also be available.
The multidisciplinary team requires administrative support in developing the agenda for the meeting, for collating patient information and to ensure appropriate expertise around the table to create an effective treatment plan for the patient. The MDM has a chair and multiple lead clinicians. Each patient case will be presented by a lead clinician (usually someone who has seen the patient before the MDM). In public hospital settings, the registrar or clinical fellow may take this role. A member of the team records the outcomes of the discussion and treatment plan in the patient history and ensures these details are communicated to the patient’s general practitioner. The team should consider the patient’s values, beliefs and cultural needs as appropriate to ensure the treatment plan is in line with these.
The multidisciplinary team should be composed of the core disciplines that are integral to providing good care. Team membership should reflect both clinical and supportive care aspects of care. Pathology and radiology expertise are essential.
See ‘About this OCP’ for a list of team members who may be included in the multidisciplinary team for pancreatic cancer.
Core members of the multidisciplinary team are expected to attend most MDMs either in person or remotely via virtual mechanisms. Additional expertise or specialist services may be required for some patients. An Aboriginal and Torres Strait Islander cultural expert should be considered for all patients who identify as Aboriginal or Torres Strait Islander.
The general practitioner who made the referral is responsible for the patient until care is passed to another practitioner who is directly involved in planning the patient’s care.
The general practitioner may play a number of roles in all stages of the cancer pathway including diagnosis, referral, treatment, shared follow-up care, post-treatment surveillance, coordination and continuity of care, as well as managing existing health issues and providing information and support to the patient, their family and carer.
A nominated contact person from the multidisciplinary team may be assigned responsibility for coordinating care in this phase. Care coordinators are responsible for ensuring there is continuity throughout the care process and coordination of all necessary care for a particular phase (COSA 2015). The care coordinator may change over the course of the pathway.
The lead clinician is responsible for overseeing the activity of the team and for implementing treatment within the multidisciplinary setting.
Patients should be encouraged to participate in research or clinical trials where available and appropriate.
For more information visit the Cancer Australia website.
Cancer prehabilitation uses a multidisciplinary approach combining exercise, nutrition and psychological strategies to prepare patients for the challenges of cancer treatment such as surgery, systemic therapy and radiation therapy. Team members may include anaesthetists, oncologists, surgeons, haematologists, clinical psychologists, exercise physiologists, physiotherapists and dietitians, among others.
Patient performance status is a central factor in cancer care and should be frequently assessed. All patients should be screened for malnutrition using a validated tool, such as the Malnutrition Screening Tool (MST). The lead clinician may refer obese or malnourished patients to a dietitian preoperatively or before other treatments begin.
Patients who currently smoke should be encouraged to stop smoking before receiving treatment. This should include an offer of referral to Quitline in addition to smoking cessation pharmacotherapy if clinically appropriate.
Evidence indicates that patients who respond well to prehabilitation may have fewer complications after treatment. For example, those who were exercising before diagnosis and patients who use prehabilitation before starting treatment may improve their physical or psychological outcomes, or both, and this helps patients to function at a higher level throughout their cancer treatment (Cormie et al. 2017; Silver 2015).
For patients with pancreatic cancer, the multidisciplinary team should consider these specific prehabilitation assessments and interventions for treatment-related complications or major side effects:
- conducting a physical and psychological assessment to establish a baseline function level
- identifying impairments and providing targeted interventions to improve the patient’s function level (Silver & Baima 2013)
- reviewing the patient’s medication to ensure optimisation and to improve adherence to medicine used for comorbid conditions.
Following completion of primary cancer treatment, rehabilitation programs have considerable potential to enhance physical function.
Cancer and cancer treatment may cause fertility problems. This will depend on the age of the patient, the type of cancer and the treatment received. Infertility can range from difficulty having a child to the inability to have a child. Infertility after treatment may be temporary, lasting months to years, or permanent (AYA Cancer Fertility Preservation Guidance Working Group 2014).
Patients need to be advised about and potentially referred for discussion about fertility preservation before starting treatment and need advice about contraception before, during and after treatment. Patients and their family should be aware of the ongoing costs involved in optimising fertility. Fertility management may apply in both men and women. Fertility preservation options are different for men and women and the need for ongoing contraception applies to both men and women.
The potential for impaired fertility should be discussed and reinforced at different time points as appropriate throughout the diagnosis, treatment, surveillance and survivorship phases of care. These ongoing discussions will enable the patient and, if applicable, the family to make informed decisions. All discussions should be documented in the patient’s medical record.
See the Cancer Council website for more information.
See validated screening tools mentioned in Principle 4 ‘Supportive care’.
A number of specific challenges and needs may arise for patients at this time:
- assistance for dealing with psychological and emotional distress while adjusting to the diagnosis; treatment phobias; existential concerns; stress; difficulties making treatment decisions; anxiety or depression or both; psychosexual issues such as potential loss of fertility and premature menopause; history of sexual abuse; and interpersonal problems
- management of physical symptoms such as pain and fatigue (Australian Adult Cancer Pain Management Guideline Working Party 2019)
- malnutrition or undernutrition, identified using a validated nutrition screening tool such as the MST (note that many patients with a high BMI [obese patients] may also be malnourished [WHO 2018])
- support for families or carers who are distressed with the patient’s cancer diagnosis
- support for families/relatives who may be distressed after learning of a genetically linked cancer diagnosis
- specific spiritual needs that may benefit from the involvement of pastoral/spiritual care.
Additionally, palliative care may be required at this stage.
For more information on supportive care and needs that may arise for different population groups, see Appendices A and B, and special population groups.
In discussion with the patient, the lead clinician should undertake the following:
- establish if the patient has a regular or preferred general practitioner and if the patient does not have one, then encourage them to find one
- provide written information appropriate to the health literacy of the patient about the diagnosis and treatment to the patient and carer and refer the patient to the Guide to best cancer care (consumer optimal care pathway) for pancreatic cancer, as well as to relevant websites and support groups as appropriate
- provide a treatment care plan including contact details for the treating team and information on when to call the hospital
- discuss a timeframe for diagnosis and treatment with the patient and carer
- discuss the benefits of multidisciplinary care and gain the patient’s consent before presenting their case at an MDM
- provide brief advice and refer to Quitline (13 7848) for behavioural intervention if the patient currently smokes (or has recently quit), and prescribe smoking cessation pharmacotherapy, if clinically appropriate
- recommend an ‘integrated approach’ throughout treatment regarding nutrition, exercise and minimal or no alcohol consumption among other considerations
- communicate the benefits of continued engagement with primary care during treatment for managing comorbid disease, health promotion, care coordination and holistic care
- where appropriate, review fertility needs with the patient and refer for specialist fertility management (including fertility preservation, contraception, management during pregnancy and of future pregnancies)
- be open to and encourage discussion about the diagnosis, prognosis (if the patient wishes to know) and survivorship and palliative care while clarifying the patient’s preferences and needs, personal and cultural beliefs and expectations, and their ability to comprehend the communication
- encourage the patient to participate in advance care planning including considering appointing one or more substitute decision-makers and completing an advance care directive to clearly document their treatment preferences. Each state and territory has different terminology and legislation surrounding advance care directives and substitute decision-makers.
The lead clinician has these communication responsibilities:
- involving the general practitioner from the point of diagnosis
- ensuring regular and timely communication with the general practitioner about the diagnosis, treatment plan and recommendations from MDMs and inviting them to participate in MDMs (consider using virtual mechanisms)
- supporting the role of general practice both during and after treatment
- discussing shared or team care arrangements with general practitioners or regional cancer specialists, or both, together with the patient.
Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
Step 4 describes the optimal treatments for pancreatic cancer, the training and experience required of the treating clinicians and the health service characteristics required for optimal cancer care.
All health services must have clinical governance systems that meet the following integral requirements:
- identifying safety and quality measures
- monitoring and reporting on performance and outcomes
- identifying areas for improvement in safety and quality (ACSQHC 2020).
Step 4 outlines the treatment options for pancreatic cancer. For detailed clinical information on treatment options refer to these resources:
- the National Comprehensive Cancer Network’s 2019 Clinical practice guidelines for pancreatic cancer
- the National Institute for Health and Care Excellence’s 2018 Pancreatic cancer in adults: diagnosis and management
- the National Cancer Institute’s 2020 Pancreatic cancer treatment (adult)(PDQ) – Health professional version
- the European Society for Medical Oncology’s 2015 Cancer of the pancreas: ESMO clinical practice guidelines and the 2019 eUpdate
The intent of treatment can be defined as one of the following:
- curative
- anti-cancer therapy to improve quality of life and/or longevity without expectation of cure
- symptom palliation.
The treatment intent should be established in a multidisciplinary setting, documented in the patient’s medical record and conveyed to the patient and carer as appropriate.
The potential benefits need to be balanced against the morbidity and risks of treatment.
The lead clinician should discuss the advantages and disadvantages of each treatment and associated potential side effects with the patient and their carer or family before treatment consent is obtained and begins so the patient can make an informed decision. Supportive care services should also be considered during this decision-making process. Patients should be asked about their use of (current or intended) complementary therapies (see Appendix D).
Timeframes for starting treatment should be informed by evidence-based guidelines where they exist. The treatment team should recognise that shorter timeframes for appropriate consultations and treatment can promote a better experience for patients.
Initiate advance care planning discussions with patients before treatment begins (this could include appointing a substitute decision-maker and completing an advance care directive). Formally involving a palliative care team/service may benefit any patient, so it is important to know and respect each person’s preference (AHMAC 2011).
The potential for curative surgery depends on the staging of the tumour, and only 10–20 per cent of patients have clearly resectable disease after careful pretherapeutic staging. This potential is assessed by the multidisciplinary team.
Patients who undergo surgical resection for localised pancreatic cancer have a median survival of 15–20 months and a five-year survival of 8–15 per cent (Lambert et al. 2019). Unfortunately, 80 per cent of patients present with metastatic or locally advanced disease, by which time the tumour is unresectable (Lambert et al. 2019).
Unresectable tumours are defined based on the presence of metastases including non-regional lymph node involvement, more than 180 degrees of contact with the major vessels, or tumoural invasion of the major vessels (Elbanna et al. 2020).
Curative surgery includes the following options with or without chemotherapy (adjuvant or neoadjuvant chemotherapy or neoadjuvant chemoradiation):
- Whipple procedure (pancreaticoduodenal resection)
- distal pancreatectomy
- total pancreatectomy.
Timeframe for starting treatment
Surgery should be undertaken within four weeks of the initial diagnosis, depending on urgency and modality.
Training and experience required of the surgeon
Surgeon (FRACS or equivalent) with adequate training and experience in hepatobiliary surgery with institutional credentialing and agreed scope of practice within this area.
There is strong evidence to suggest that surgeons who undertake a high volume of resections have better clinical outcomes for complex cancer surgery such as pancreatic resections (Toomey et al. 2016).
Documented evidence of the surgeon’s training and experience, including their specific (sub-specialty) experience with pancreatic cancer and procedures to be undertaken, should be available.
Health service characteristics
To provide safe and quality care for patients having surgery, health services should have these features:
- critical care support
- 24-hour medical staff availability
- 24-hour operating room access and intensive care unit
- diagnostic imaging
- endoscopic retrograde cholangiopancreatography (ERCP)
- 24-hour access to interventional radiology
- access to endoscopic ultrasound
- nuclear medicine imaging
- pathology
- full support from other surgical specialties.
There is strong evidence to suggest that high-volume hospitals have better clinical outcomes for complex cancer surgery such as pancreatic resections (Hata et al. 2016). Centres that do not have sufficient caseloads should establish processes to routinely refer surgical cases to high-volume centres.
Even if the cancer is deemed surgically curable the following should be considered (NCI 2019a):
- neoadjuvant chemotherapy for all high-risk patients
- neoadjuvant chemotherapy or chemoradiation therapy, especially in patients with borderline resectable disease or delay in surgery
- adjuvant chemotherapy in the postoperative setting
- chemoradiation therapy (or SBRT on a trial) for borderline resectable or locally advanced patients who are still potentially operable
- adjuvant chemotherapy within 12 weeks following resection.
Timeframes for starting treatment
Neoadjuvant chemotherapy should begin within four weeks of the initial diagnosis, depending on urgency and modality.
Adjuvant chemotherapy in the postoperative setting should begin within 12 weeks of surgery.
Training and experience required of the appropriate specialists
Medical oncologists must have training and experience of this standard:
- Fellow of the Royal Australian College of Physicians (or equivalent)
- adequate training and experience that enables institutional credentialing and agreed scope of practice within this area (ACSQHC 2015).
Cancer nurses should have accredited training in these areas:
- anti-cancer treatment administration
- specialised nursing care for patients undergoing cancer treatments, including side effects and symptom management
- the handling and disposal of cytotoxic waste (ACSQHC 2020).
Systemic therapy should be prepared by a pharmacist whose background includes this experience:
- adequate training in systemic therapy medication, including dosing calculations according to protocols, formulations and/or preparation.
In a setting where no medical oncologist is locally available (e.g. regional or remote areas), some components of less complex therapies may be delivered by a general practitioner or nurse with training and experience that enables credentialing and agreed scope of practice within this area. This should be in accordance with a detailed treatment plan or agreed protocol, and with communication as agreed with the medical oncologist or as clinically required.
The training and experience of the appropriate specialist should be documented.
Health service characteristics (systemic therapy)
To provide safe and quality care for patients having systemic therapy, health services should have these features:
- a clearly defined path to emergency care and advice after hours
- access to diagnostic pathology including basic haematology and biochemistry, and imaging
- cytotoxic medicines prepared in a pharmacy with appropriate facilities or externally sourced from Therapeutics Goods Association–licensed manufacturers
- occupational health and safety guidelines regarding handling of cytotoxic drugs, including preparation, waste procedures and spill kits (eviQ 2019;)
- guidelines and protocols to deliver treatment safely (including dealing with extravasation of drugs)
- coordination for combined therapy with radiation therapy, especially where facilities are not co-located
- appropriate molecular pathology access.
Training and experience required of radiation oncologists
Radiation oncologists must have training and experience of this standard:
- Fellowship of the Royal Australian and New Zealand College of Radiologists (or equivalent)
- adequate training and experience, institutional credentialing and agreed scope of practice in pancreatic cancer (ACSQHC 2015).
The training and experience of the radiation oncologist should be documented.
Health service unit characteristics (radiation therapy)
To provide safe and quality care for patients having radiation therapy, health services should have these features:
- linear accelerator (LINAC) capable of image-guided radiation therapy (IGRT)
- dedicated CT planning
- access to MRI and PET imaging
- automatic record-verify of all radiation treatments delivered
- a treatment planning system
- trained medical physicists, radiation therapists and nurses with radiation therapy experience
- coordination for combined therapy with systemic therapy, especially where facilities are not co-located
- participation in Australian Clinical Dosimetry Service audits
- an incident management system linked with a quality management system.
If the cancer is deemed unresectable, any other treatment is almost certainly palliative because pancreatic cancer is unlikely to be cured by chemotherapy and radiation therapy. Palliative therapy may be indicated for:
- nutritional assessment and support (including enzyme support therapy)
- surgical or radiological biliary decompression
- relief of gastric outlet obstruction
- pain control
- psychological care to address the potentially disabling psychological events associated with the diagnosis and treatment of pancreatic cancer.
The most commonly used therapies in unresectable pancreatic cancer include:
- endoscopic or radiological intervention
- surgical interventions – endoscopic biliary stent placement, percutaneous radiological biliary stent placement, palliative surgical biliary and/or gastric bypass
- chemotherapy
- chemotherapy followed by chemoradiation therapy for those without metastatic disease
- chemotherapy, followed by radiotherapy in selected cases
- coeliac plexus or intrapleural block.
For patients who are too unwell to undergo curative therapy, radiotherapy has been shown to improve survival, pain control and hospital admissions compared with the best supportive care.
Endoscopic stenting is recommended as initial palliation for biliary obstruction. Percutaneous transhepatic biliary stenting may be required for failed endoscopic stenting. For patients with gastric outlet obstruction, either surgical bypass or endoscopic stenting would be appropriate.
It is important to weigh up the risks versus benefits of any palliative therapy if the patient’s prognosis is not changed with implementation.
Timeframes for starting treatment
Treatment should begin within four weeks of initial diagnosis, depending on urgency and modality.
There is currently one approved targeted therapy available to treat patients with locally advanced, unresectable or metastatic pancreatic cancer.
Maintenance therapy with the PARP inhibitor olaparib (Lynparza) has been shown to significantly delay the progression of metastatic pancreatic cancer in patients with BRCA gene mutations compared with placebo (ASCO 2019).
A number of emerging therapies are being investigated for pancreatic cancer. Areas of interest for emerging therapies include identifying molecular targets, targeting cancer stem cells and stromal modulation, immunotherapies such as cancer vaccines, adoptive cell therapy and stemness inhibitors (Amanam & Chung 2018; Lambert et al. 2019).
The key principle for precision medicine is prompt and clinically oriented communication and coordination with an accredited laboratory and pathologist. Tissue analysis is integral for access to emerging therapies and, as such, tissue specimens should be treated carefully to enable additional histopathological or molecular diagnostic tests in certain scenarios.
Early referral to palliative care can improve the quality of life for people with cancer (Haines 2011; Temel at al. 2010; Zimmermann et al. 2014). This is particularly true for cancers with poor prognosis.
In general, all patients with pancreatic cancer, given the poor prognosis, should be offered referral to palliative care assessment as an integrated aspect of their overall oncology care (Gaertner et al. 2011).
In particular, referral to palliative care services is required when:
- symptoms affect quality of life
- ECOG ≥ 2
- estimated likely survival is less than a year and/or the patient/carer has increasing difficulty managing care needs
- complex psychosocial needs, including those of carers
- patient/family wishes for palliative care support, especially in the community setting
- bereavement support for carers.
Emphasise the value of palliative care in improving symptom management and quality of life to patients and their carers.
The ‘Dying to Talk’ resource may help health professionals when initiating discussions with patients about future care needs (see ‘More information’). Ensure that carers and families receive information, support and guidance about their role in palliative care (Palliative Care Australia 2018).
Patients, with support from their family or carer and treating team, should be encouraged to consider appointing a substitute decision-maker and to complete an advance care directive.
Refer to Step 6 for a more detailed description of managing patients with recurrent, residual or metastatic disease.
These online resources are useful:
The team should support the patient to participate in research or clinical trials where available and appropriate. Many emerging treatments are only available on clinical trials that may require referral to certain trial centres.
For more information visit the Cancer Australia website.
See validated screening tools mentioned in Principle 4 ‘Supportive care’.
A number of specific challenges and needs may arise for patients at this time:
- assistance for dealing with emotional and psychological issues, including body image concerns, fatigue, quitting smoking, traumatic experiences, existential anxiety, treatment phobias, anxiety/depression, interpersonal problems and sexuality concerns
- potential isolation from normal support networks, particularly for rural patients who are staying away from home for treatment
- management of physical symptoms such as chronic pain and fatigue
- nutritional assessment and support
- gastrointestinal symptoms (such as nausea, vomiting, mucositis, loss of appetite) as a result of chemotherapy treatment, requiring optimal symptom control with medication and referral to a dietitian if dietary intake is affected
- assistance with managing complex medication regimens, multiple medications, assessment of side effects and assistance with difficulties swallowing medications – referral to a pharmacist may be required
- decline in mobility or functional status as a result of treatment
- assistance with beginning or resuming regular exercise with referral to an exercise physiologist or physiotherapist (COSA 2018; Hayes et al. 2019).
Early involvement of general practitioners may lead to improved cancer survivorship care following acute treatment. General practitioners can address many supportive care needs through good communication and clear guidance from the specialist team (Emery 2014).
Patients, carers and families may have these additional issues and needs:
- financial issues related to loss of income (through reduced capacity to work or loss of work) and additional expenses as a result of illness or treatment
- advance care planning, which may involve appointing a substitute decision-maker and completing an advance care directive
- legal issues (completing a will, care of dependent children) or making an insurance, superannuation or social security claim on the basis of terminal illness or permanent disability.
Cancer Council’s 13 11 20 information and support line can assist with information and referral to local support services.
For more information on supportive care and needs that may arise for different population groups, see Appendices A and B, and special population groups.
Rehabilitation may be required at any point of the care pathway. If it is required before treatment, it is referred to as prehabilitation (see section 3.6.1).
All members of the multidisciplinary team have an important role in promoting rehabilitation. Team members may include occupational therapists, speech pathologists, dietitians, social workers, psychologists, physiotherapists, exercise physiologists and rehabilitation specialists.
To maximise the safety and therapeutic effect of exercise for people with cancer, all team members should recommend that people with cancer work towards achieving, and then maintaining, recommended levels of exercise and physical activity as per relevant guidelines. Exercise should be prescribed and delivered under the direction of an accredited exercise physiologist or physiotherapist with experience in cancer care (Vardy et al. 2019). The focus of intervention from these health professionals is tailoring evidence-based exercise recommendations to the individual patient’s needs and abilities, with a focus on the patient transitioning to ongoing self-managed exercise.
Other issues that may need to be dealt with include managing cancer-related fatigue, improving physical endurance, achieving independence in daily tasks, optimising nutritional intake, returning to work and ongoing adjustment to cancer and its sequels. Referrals to dietitians, psychosocial support, return-to-work programs and community support organisations can help in managing these issues.
The lead or nominated clinician should take responsibility for these tasks:
- discussing treatment options with patients and carers, including the treatment intent and expected outcomes, and providing a written version of the plan and any referrals
- providing patients and carers with information about the possible side effects of treatment, managing symptoms between active treatments, how to access care, self-management strategies and emergency contacts
- encouraging patients to use question prompt lists and audio recordings, and to have a support person present to aid informed decision making
- initiating a discussion about advance care planning and involving carers or family if the patient wishes
The general practitioner plays an important role in coordinating care for patients, including helping to manage side effects and other comorbidities, and offering support when patients have questions or worries. For most patients, simultaneous care provided by their general practitioner is very important.
The lead clinician, in discussion with the patient’s general practitioner, should consider these points:
- the general practitioner’s role in symptom management, supportive care and referral to local services
- using a chronic disease management plan and mental health care management plan
- how to ensure regular and timely two-way communication about:
- the treatment plan, including intent and potential side effects
- supportive and palliative care requirements
- the patient’s prognosis and their understanding of this
- enrolment in research or clinical trials
- changes in treatment or medications
- the presence of an advance care directive or appointment of a substitute decision-maker
- recommendations from the multidisciplinary team.
Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
The term ‘cancer survivor’ describes a person living with cancer, from the point of diagnosis until the end of life. Survivorship care in Australia has traditionally been provided to patients who have completed active treatment and are in the post-treatment phase. But there is now a shift to provide survivorship care and services from the point of diagnosis to improve cancer-related outcomes.
Cancer survivors may experience inferior quality of life and cancer-related symptoms for up to five years after their diagnosis (Jefford et al. 2017). Distress, fear of cancer recurrence, fatigue, obesity and sedentary lifestyle are common symptoms reported by cancer survivors (Vardy et al. 2019).
Due to an ageing population and improvements in treatments and supportive care, the number of people surviving cancer is increasing. International research shows there is an important need to focus on helping cancer survivors cope with life beyond their acute treatment. Cancer survivors often face issues that are different from those experienced during active treatment for cancer and may include a range of issues, as well as unmet needs that affect their quality of life (Lisy et al. 2019; Tan et al. 2019).
Physical, emotional and psychological issues include fear of cancer recurrence, cancer-related fatigue, pain, distress, anxiety, depression, cognitive changes and sleep issues (Lisy et al. 2019). Late effects may occur months or years later and depend on the type of cancer treatment. Survivors and their carers may experience impacted relationships and practical issues including difficulties with return to work or study and financial hardship. They may also experience changes to sex and intimacy. Fertility, contraception and pregnancy care after treatment may require specialist input.
The Institute of Medicine, in its report From cancer patient to cancer survivor: Lost in transition, describes the essential components of survivorship care listed in the paragraph above, including interventions and surveillance mechanisms to manage the issues a cancer survivor may face (Hewitt et al. 2006). Access to a range of health professions may be required including physiotherapy, occupational therapy, social work, dietetics, clinical psychology, fertility and palliative care. Coordinating care between all providers is essential to ensure the patient’s needs are met.
Cancer survivors are more likely than the general population to have and/or develop comorbidities (Vijayvergia & Denlinger 2015). Health professionals should support survivors to self-manage their own health needs and to make informed decisions about lifestyle behaviours that promote wellness and improve their quality of life (Australian Cancer Survivorship Centre 2016; Cancer Australia 2017b; NCSI 2015).
The transition from active treatment to post-treatment care is critical to long-term health. In some cases, people will need ongoing, hospital-based care, and in other cases a shared follow-up care arrangement with their general practitioner may be appropriate. This will vary depending on the type and stage of cancer and needs to be planned.
Shared follow-up care involves the joint participation of specialists and general practitioners in the planned delivery of follow-up and survivorship care. A shared care plan is developed that outlines the responsibilities of members of the care team, the follow-up schedule, triggers for review, plans for rapid access into each setting and agreement regarding format, frequency and triggers for communication.
After completing initial treatment, a designated member of the multidisciplinary team (most commonly nursing or medical staff involved in the patient’s care) should provide the patient with a needs assessment and treatment summary and develop a survivorship care plan in conjunction with the patient. This should include a comprehensive list of issues identified by all members of the multidisciplinary team involved in the patient’s care and by the patient. These documents are key resources for the patient and their healthcare providers and can be used to improve communication and care coordination.
The treatment summary should cover, but is not limited to:
- the diagnostic tests performed and results
- diagnosis including stage, prognostic or severity score
- tumour characteristics
- treatment received (types and dates)
- current toxicities (severity, management and expected outcomes)
- interventions and treatment plans from other health providers
- potential long-term and late effects of treatment
- supportive care services provided
- follow-up schedule
- contact information for key healthcare providers
As most patients with pancreatic cancer are palliated, they should already have a palliative care physician/team that will oversee their palliation. If a patient is thought to have been cured after their treatment, then care in the post-treatment phase is driven by predicted risks (such as the risk of recurrence, developing late effects and psychological issues) as well as individual clinical and supportive care needs. It is important that post-treatment care is evidence-based and consistent with guidelines. Currently there is no established protocol for postoperative surveillance.
Follow-up care over the first two years should be based on institutional experience. Ideally, three–six-monthly tumour markers and radiological imaging should be carried out for patients at high risk of developing a new pancreatic cancer.
Responsibility for follow-up care should be agreed between the lead clinician, the general practitioner, relevant members of the multidisciplinary team and the patient. This is based on guideline recommendations for post-treatment care, as well as the patient’s current and anticipated physical and emotional needs and preferences.
Evidence comparing shared follow-up care and specialised care indicates equivalence in outcomes including recurrence rate, cancer survival and quality of life (Cancer Research in Primary Care 2016).
Ongoing communication between healthcare providers involved in care and a clear understanding of roles and responsibilities is key to effective survivorship care.
In particular circumstances, other models of post-treatment care can be safely and effectively provided such as nurse-led models of care (Monterosso et al. 2019). Other models of post-treatment care can be provided in these locations or by these health professionals:
- in a shared care setting
- in a general practice setting
- by non-medical staff
- by allied health or nurses
- in a non-face-to-face setting (e.g. by telehealth).
A designated member of the team should document the agreed survivorship care plan. The survivorship care plan should support wellness and have a strong emphasis on healthy lifestyle changes such as a balanced diet, a non-sedentary lifestyle, weight management and a mix of aerobic and resistance exercise (COSA 2018; Hayes et al. 2019).
This survivorship care plan should also cover, but is not limited to:
- what medical follow-up is required (surveillance for recurrence or secondary and metachronous cancers, screening and assessment for medical and psychosocial effects)
- model of post-treatment care, the health professional providing care and where it will be delivered
- care plans from other health providers to manage the consequences of cancer and cancer treatment
- wellbeing, primary and secondary prevention health recommendations that align with chronic disease management principles
- rehabilitation recommendations
- available support services
- a process for rapid re-entry to specialist medical services for suspected recurrence.
The survivorship care plan may need to be updated to reflect changes in the patient’s clinical and psychosocial status and needs.
Processes for rapid re-entry to hospital care should be documented and communicated to the patient and relevant stakeholders.
The lead clinician should discuss (and general practitioner reinforce) options for follow-up at the start and end of treatment. It is critical for optimal aftercare that the designated member of the treatment team educates the patient about the symptoms of recurrence.
General practitioners (including nurses) can:
- connect patients to local community services and programs
- manage long-term and late effects
- manage comorbidities
- provide wellbeing information and advice to promote self-management
- screen for cancer and non-cancerous conditions.
Templates and other resources to help with developing treatment summaries and survivorship care plans are available from these organisations:
- Australian Cancer Survivorship Centre
- Cancer Australia – Principles of Cancer Survivorship
- Cancer Council Australia and states and territories
- Clinical Oncology Society of Australia – Model of Survivorship Care
- eviQ – Cancer survivorship: introductory course
- MyCarePlan.org.au
- South Australian Cancer Service – Statewide Survivorship Framework resources
- American Society of Clinical Oncology – guidelines
Not smoking, eating a healthy diet, being sun smart, avoiding or limiting alcohol intake, being physically active and maintaining a healthy body weight may help reduce the risk of primary recurrence or a second primary cancer.
Encourage and support all cancer survivors to reduce modifiable risk factors for recurrence as well as other chronic diseases. Ongoing coordination of care between providers should also deal with any comorbidities, particularly ongoing complex and life-threatening comorbid conditions.
Support cancer survivors to participate in research or clinical trials where they are available and appropriate. These might include studies to understand survivors’ issues, to better manage treatment side effects, or to improve models of care and quality of life.
For more information visit the Cancer Australia website.
See validated screening tools mentioned in Principle 4 ‘Supportive care’. Additionally, the ‘Cancer Survivors Unmet Needs (CaSun)’ is another validated screening tool that may help health professionals to identify the unmet needs of patients during survivorship.
A number of specific challenges and needs may arise for cancer survivors:
- nutritional assessment and support (including post-surgical enzyme support therapy)
- malnutritional post-treatment side effects (such as weight loss, reduced oral intake); this requires monitoring and nutrition intervention where indicated – validated malnutrition screening tools (such as MST) should be used at the key points in the care pathway to identify patients at risk of malnutrition (Loeliger & Dewar 2019)
- decline in mobility and/or functional status as a result of treatment
- a need for increased community supports as patients recover from treatment
- financial and employment issues (such as loss of income and assistance with returning to work, and the cost of treatment, travel and accommodation)
- appointing a substitute decision-maker and completing an advance care directive
- legal issues such as completing a will.
For more information on supportive care and needs that may arise for different population groups, see Appendices A and B, and special population groups.
Rehabilitation may be required at any point of the care pathway from the pre-treatment phase through to disease-free survival and palliative care (Cormie et al. 2017).
Issues that may need to be dealt with include managing cancer-related fatigue, coping with cognitive changes, improving physical endurance, achieving independence in daily tasks, returning to study or work and ongoing adjustment to cancer and its sequels.
Exercise is a safe and effective intervention that improves the physical and emotional health and wellbeing of cancer patients. Exercise should be embedded as part of standard practice in cancer care and be viewed as an adjunct therapy that helps counteract the adverse effects of cancer and its treatment.
Cancer survivors may find referral to specific cancer rehabilitation, optimisation programs or community-based rehabilitation appropriate and beneficial. Other options include referral to allied health supports through team care arrangements and mental health plans. Some community support organisations (cancer-related non-government, not-for-profit and charities) provide services to cancer survivors.
The lead clinician (themselves or by delegation) should take responsibility for these tasks:
- explaining the model of post-treatment care and the roles of health professionals involved in post-treatment care including the role of general practice
- explaining the treatment summary and follow-up care plan
- discussing the development of a shared follow-up and survivorship care plan where a model of shared follow-up care has been agreed
- discussing how to manage any of the physical, psychological or emotional issues identified
- providing information on the signs and symptoms of recurrent disease
- providing a survivorship care plan with information on secondary prevention and healthy living
- providing contact details of the care team involved
- providing clear information about the role and benefits of palliative care and advance care planning
The lead clinician should ensure regular, timely, two-way communication with the general practitioner about:
- the patient’s progress
- the follow-up care plan
- potential late effects
- supportive and palliative care requirements
- any shared care arrangements
- clarification of various roles in patient care
- a process for rapid re-entry to medical services for patients with suspected recurrence or if there are other concerns.
Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
Patients who present with recurrent, residual or metastatic disease should be managed by a multidisciplinary team and offered timely referral to appropriate physical, practical and emotional support.
Step 6 is concerned with managing recurrent or local residual and metastatic disease. The likelihood of recurrence depends on many factors usually related to the type of cancer, the stage of cancer at presentation and the effectiveness of treatment. Some cancers cannot be eradicated even with the best initial treatment. But controlling disease and disease-related symptoms is sometimes possible, depending on the clinical situation.
With the low rates of curable pancreatic cancer and the majority of patients palliated, it is likely that their current symptoms will worsen progressively, and this should be managed following discussion by a multidisciplinary team in consultation with palliative care specialists.
Some patients will have metastatic disease on initial presentation. Others may present with symptoms of recurrent disease after a previous cancer diagnosis. Access to the best available therapies, including clinical trials, as well as treatment overseen by a multidisciplinary team, are crucial to achieving the best outcomes for anyone with metastatic disease.
Signs and symptoms will depend on the type of cancer initially diagnosed and the location of metastatic disease. They may be discovered by the patient or by surveillance in the post-treatment period. Symptoms can often present as weight loss, jaundice and abdominal pain.
Managing metastatic disease is complex and should therefore involve all the appropriate specialties in a multidisciplinary team including palliative care where appropriate. From the time of diagnosis, the team should offer patients appropriate psychosocial care, supportive care, advance care planning and symptom-related interventions as part of their routine care. The approach should be personalised to meet the patient’s individual needs, values and preferences. The full complement of supportive care measures as described throughout the optimal care pathway and in Appendices A and B, and in the special population groups section should be offered to assist patients and their families and carers to cope. These measures should be updated as the patient’s circumstances change.
Survivorship care should be considered and offered at an early stage. Some people live with advanced cancer for many months or years. As survival is improving in many patients, survivorship issues should be considered as part of routine care. Health professionals should therefore be ready to change and adapt treatment strategies according to disease status, prior treatment tolerance and toxicities and the patient’s quality of life, in addition to the patient’s priorities and life plans.
If there is an indication that a patient’s cancer has returned, care should be provided under the guidance of a treating specialist. Each patient should be evaluated to determine if referral to the original multidisciplinary team is necessary. Often referral back to the original multidisciplinary team will not be necessary unless there are obvious aspects of care involving different therapeutic and supportive care disciplines not otherwise accessible. The multidisciplinary team may include new members such as palliative care specialists.
Treatment will depend on the location, extent of recurrent or residual disease, previous management and the patient’s preferences.
In managing people with pancreatic cancer, treatment may include these options:
- surgery
- stenting
- chemotherapy
- radiation therapy
- intra-arterial therapies
- percutaneous ablation
- pain management
- palliative care.
The potential goals of treatment should be discussed, respecting the patient’s cultural values. Wherever possible, written information should be provided.
Encourage early referral to clinical trials or accepting an invitation to participate in research.
Advance care planning is important for all patients with a cancer diagnosis but especially those with advanced disease. Patients should be encouraged to think and talk about their healthcare values and preferences with family or carers, appoint a substitute decision-maker and consider developing an advance care directive to convey their preferences for future health care in the event they become unable to communicate their wishes (AHMAC 2011).
Refer to section 4.3 ‘More information’ for links to resources.
Refer patients and carers to Advance Care Planning Australia or to the Advance Care Planning National Phone Advisory Service on 1300 208 582.
Early referral to palliative care has been shown to improve the quality of life for people with cancer (Haines 2011; Temel et al. 2010; Zimmermann et al. 2014). In general, all patients with pancreatic cancer, given the poor prognosis, should be offered referral to palliative care assessment as an integrated aspect of their overall oncology care (Gaertner et al. 2011). The treatment team should emphasise the value of palliative care in improving symptom management and quality of life to patients and their carers. Refer to section 4.3 for more detailed information.
The lead clinician should ensure timely and appropriate referral to palliative care services.
Refer to the end of section 4.3 ‘Palliative care’ for links to resources.
The treatment team should support the patient to participate in research and clinical trials where available and appropriate.
For more information visit the Cancer Australia website.
See validated screening tools mentioned in Principle 4 ‘Supportive care’.
A number of specific challenges and needs may arise at this time for patients:
- assistance for dealing with emotional and psychological distress resulting from fear of death or dying, existential concerns, anticipatory grief, communicating wishes to loved ones, interpersonal problems and sexuality concerns
- potential isolation from normal support networks, particularly for rural patients who are staying away from home for treatment
- cognitive changes as a result of treatment and disease progression such as altered memory, attention and concentration (a patient may appoint someone to make medical, financial and legal decisions on their behalf – a substitute decision-maker – before and in case they experience cognitive decline)
- management of physical symptoms including pain and fatigue
- nutritional assessment and support (including enzyme support therapy)
- decline in mobility or functional status as a result of recurrent disease and treatments (referral to physiotherapy or occupational therapy may be required)
- coping with hair loss and changes in physical appearance (refer to the Look Good, Feel Better program– see ’Resource List’)
- appointing a substitute decision-maker and completing an advance care directive
- financial issues as a result of disease recurrence such as gaining early access to superannuation and insurance
- legal issues (completing a will, care of dependent children) and making an insurance, superannuation or social security claim on the basis of terminal illness or permanent disability.
Rehabilitation may be required at any point of the metastatic care pathway, from preparing for treatment through to palliative care. Issues that may need to be dealt with include managing cancer-related fatigue, improving physical endurance, achieving independence in daily tasks, returning to work and ongoing adjustment to cancer and its sequels.
Exercise is a safe and effective intervention that improves the physical and emotional health and wellbeing of cancer patients. Exercise should be embedded as part of standard practice in cancer care and be viewed as an adjunct therapy that helps counteract the adverse effects of cancer and its treatment.
The lead clinician should ensure there is adequate discussion with patients and carers about the diagnosis and recommended treatment, including treatment intent and possible outcomes, likely adverse effects and the supportive care options available.
Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
Step 7 is concerned with maintaining the patient’s quality of life and meeting their health and supportive care needs as they approach the end of life, as well as the needs of their family and carers.
Some patients with advanced cancer will reach a time when active treatment is no longer appropriate. The team needs to share the principles of a palliative approach to care when making decisions with the patient and their family or carer. End-of-life care is appropriate when the patient’s symptoms are increasing and functional status is declining.
If the treatment team does not include a palliative care member, the lead clinician should consider referring the patient to palliative care services, with the general practitioner’s engagement. This may include inpatient palliative unit access (as required).
The multidisciplinary team may consider seeking additional expertise from these professionals:
- clinical psychologist
- clinical nurse specialist or practitioner
- social worker
- palliative medicine specialist
- pain specialist
- pastoral or spiritual carer
- bereavement counsellor
- music therapist
- art therapist
- cultural expert
- Canteen for children of parents with cancer
The team might also recommend that patients access these services:
- home and community-based care
- specialist community palliative care workers
- community nursing.
If the patient does not already have an advance care directive in place, a designated member of the treatment team should encourage them to develop one in collaboration with their family or carer (AHMAC 2011).
It is essential for the treatment team to consider the appropriate place of care, the patient’s preferred place of death and the support needed for the patient, their family and carers.
The treatment team should also ensure that carers and families receive the information, support and guidance about their role according to their needs and wishes (Palliative Care Australia 2018).
The treatment team can refer patients and carers to these resources:
- Palliative Care Australia
- Advance Care Planning Australia or to Advance Care Planning Australia’s National Advisory Service on 1300 208 582.
Clinical trials may help improve palliative care and in managing a patient’s symptoms of advanced cancer (Cancer Council Victoria 2019). The treatment team should support the patient to participate in research and clinical trials where available and appropriate.
For more information visit the Cancer Australia website. See ’Resource list’ for additional clinical trial databases.
See validated screening tools mentioned in Principle 4 ‘Supportive care’.
A number of specific challenges and needs may arise for patients at this time:
- assistance for dealing with emotional and psychological distress from anticipatory grief, fear of death or dying, anxiety/depression and interpersonal problems
- management of physical symptoms including pain and fatigue
- nutritional assessment and support (including enzyme support therapy)
- decline in mobility or functional status, affecting the patient’s discharge destination (a referral to physiotherapy, exercise physiology, occupational therapy or social work may be needed)
- appointing a substitute decision-maker and completing an advance care directive
- legal issues (completing a will, care of dependent children) and making an insurance, superannuation or social security claim on the basis of terminal illness or permanent disability
- specific support for families where a parent is dying and will leave behind bereaved children or adolescents, creating special family needs
- arranging a funeral.
These services and resources can help:
- referral to 13 11 20 for Cancer Council Australia’s Pro Bono Program for free legal, financial, small business accounting and workplace assistance (subject to a means test)
- Sad news sorry business (Queensland Health 2015) for the specific needs of Aboriginal and Torres Strait Islander people.
For more information on supportive care and needs that may arise for different population groups, see Appendices A and B, and special population groups.
The lead clinician is responsible for:
- being open to and encouraging discussion with the patient about the expected disease course, considering the patient’s personal and cultural beliefs and expectations
- discussing palliative care options, including inpatient and community-based services as well as dying at home and subsequent arrangements
- providing the patient and carer with the contact details of a palliative care service
- referring the patient to palliative care in the community according to the carer’s wishes.
The lead clinician should discuss end-of-life care planning to ensure the patient’s needs and goals are met in the appropriate environment. The patient’s general practitioner should be kept fully informed and involved in major developments in the patient’s illness path.
For support with communication skills and training programs, see these sources:
The burden of cancer is not evenly spread across Australia. People experiencing socioeconomic disadvantage, Aboriginal and Torres Strait Islander communities, culturally diverse communities, people living with a disability, people with chronic mental health or psychiatric concerns and those who live in regional and rural areas of Australia have poorer cancer outcomes.
Cancer is the third leading cause of burden of disease for Aboriginal and Torres Strait Islander people. While Australia’s cancer survival rates are among the best in the world, Aboriginal and Torres Strait Islander people continue to experience a different pattern of cancer incidence and significant disparities in cancer outcomes compared with non-Indigenous Australians.
For Aboriginal and Torres Strait Islander people, health and connection to land, culture, community and identity are intrinsically linked. Health encompasses a whole-of-life view and includes a cyclical concept of life–death–life.
The distinct epidemiology of cancer among Aboriginal and Torres Strait Islander people, and unique connection to culture, highlight the need for a specific optimal care pathway for Aboriginal and Torres Strait Islander people with cancer. Ensuring this pathway is culturally safe and supportive is vital to tackling the disparities for Aboriginal and Torres Strait Islander people.
Published in 2018, the Optimal care pathway for Aboriginal and Torres Strait Islander people with cancer provides guidance to health practitioners and service planners on optimal care for Aboriginal and Torres Strait Islander people with cancer across the cancer continuum.
In addition to the key principles underpinning cancer-specific pathways, these are the key concepts that are fundamental to Aboriginal and Torres Strait Islander health:
- providing a holistic approach to health and wellbeing
- providing a culturally appropriate and culturally safe service
- acknowledging the diversity of Aboriginal and Torres Strait Islander peoples
- understanding the social determinants and cultural determinants of health (Cancer Australia 2015).
To view the Optimal care pathway for Aboriginal and Torres Strait Islander people with cancer, visit the Cancer Australia website. To view the consumer resources – Checking for cancer and Cancer, visit the Cancer Australia website.
For people from culturally diverse backgrounds in Australia, a cancer diagnosis can come with additional complexities, particularly when English proficiency is poor. In many languages there is not a direct translation of the word ‘cancer’, which can make communicating vital information difficult. Perceptions of cancer and related issues can differ greatly in people from culturally diverse backgrounds and this can affect their understanding and decision making after a cancer diagnosis. In addition to different cultural beliefs, when English language is limited there is potential for miscommunication of important information and advice, which can lead to increased stress and anxiety for patients.
A professionally trained interpreter (not a family member or friend) should be made available when communicating with people with limited English proficiency. Navigation of the Australian healthcare system can pose problems for those with a non-Anglo culture, and members of the treatment teams should pay particular attention to supporting these patients.
The Australian Cancer Survivorship Centre has developed a glossary of more than 700 cancer terms in nine different languages. The multilingual glossary has been designed as a resource for professional translators, interpreters and bilingual health professionals working in the cancer field. The glossary is a unique tool that enables language professionals with access to accurate, consistent and culturally appropriate terminology.
Visit the Peter Mac website to see the glossary.
Disability, which can be physical, intellectual or psychological, may have existed before the cancer diagnosis or may be new in onset (occurring due to the cancer treatment or incidentally). Adjusting to life with a disability adds another challenge to cancer care and survivorship.
Several barriers prevent people with disabilities from accessing timely and effective health care (AIHW 2017b):
- physical limitations
- competing health needs
- the trauma of undergoing invasive procedures
- potential barriers associated with obtaining informed consent
- failure to provide assistance with communication
- lack of information
- discriminatory attitudes among healthcare staff.
In caring for people with disabilities and a cancer diagnosis, the Australian Institute of Health and Welfare disability flag should be used at the point of admittance to correctly identify and meet the additional requirements of a person with disability. Facilities should actively consider access requirements, and health practitioners should make reasonable adjustments where required.
Patients aged between seven and 65 years who have a permanent or significant disability may be eligible for support or funding through the National Disability Insurance Scheme (National Disability Insurance Agency 2018). More information can be found on the NDIS website.
Patients aged 65 years or older (50 years or older for Aboriginal or Torres Strait Islander people) may be eligible for subsidised support and services through aged care services. An application to determine eligibility can be completed online over the phone. More information can be found at the My Aged Care website.
‘Talking End of Life’ is a resource that shows how to teach people with intellectual disability about end of life. It is designed for disability support workers but is also helpful for others including families, health professionals and educators.
To view the resource, visit the Talking End of Life website.
Given the average age at diagnosis of pancreatic cancer is 72.8 years (AIHW 2017a) , most people with pancreatic cancer are elderly and may therefore experience a rapid deterioration. Their ability to self-care may be impaired and therefore they may require early consideration of palliative care.
Planning and delivering appropriate cancer care for older people can present a number of challenges. This could also be true for frail people or those experiencing comorbidities. Effective communication between oncology and geriatrics departments will help facilitate best practice care, which takes into account physiological age, complex comorbidities, risk of adverse events and drug interactions, as well as the implications of cognitive impairment on suitability of treatment and consent (Steer et al. 2009).
At a national interdisciplinary workshop convened by the Clinical Oncology Society of Australia, it was recommended that people over the age of 70 undergo some form of geriatric assessment, in line with international guidelines (COSA 2013; palliAGED 2018). Screening tools can be used to identify those patients in need of a comprehensive geriatric assessment (Decoster et al. 2015). This assessment can be used to help determine life expectancy and treatment tolerance and guide appropriate referral for multidisciplinary intervention that may improve outcomes (Wildiers et al. 2014).
Frailty is not captured through traditional measures of performance status (e.g. ECOG) and includes assessment in the domains of:
- function
- comorbidity
- presence of geriatric syndromes
- nutrition
- polypharmacy
- cognition
- emotional status
- social supports.
Malignant pancreatic tumours are rare in children and adolescents, with an incidence of 0.46 cases per one million (younger than 30 years; NCI 2019b). In recent years, adolescent and young adult oncology has emerged as a distinct field due to lack of progress in survival and quality-of-life outcomes (Ferrari et al. 2010; Smith et al. 2013). The significant developmental change that occurs during this life stage complicates a diagnosis of cancer, often leading to unique physical, social and emotional effects for young people at the time of diagnosis and throughout the cancer journey (Smith et al. 2012).
In caring for young people with cancer, akin to the comorbidities that require specific care in the older cancer population, the treatment team needs to pay careful attention to promoting normal development (COSA 2014). This requires personalised assessments and management involving a multidisciplinary, disease-specific, developmentally targeted approach that adheres to the following principles:
- understanding the developmental stages of adolescence and supporting normal adolescent health and development alongside cancer management
- understanding and supporting the rights of young people
- communication skills and information delivery that are appropriate to the young person
- meeting the needs of all involved, including the young person, their carers and their family
- working with educational institutions and workplaces
- considering survivorship and palliative care needs.
An oncology team caring for an adolescent or young adult with cancer should be able to demonstrate these specific areas of expertise:
- be able to ensure access to expert adolescent and young adult health providers who have knowledge specific to the biomedical and psychosocial needs of the population
- understand the biology and current management of the disease in the adolescent and young adult age group
- consider participating in research and clinical trials for each patient
- engage in proactive discussion and management of fertility preservation, late effects of treatment, ongoing need for contraception, and psychosocial and psychosexual needs
- provide treatment in an environment that is friendly to adolescents and young adults.
In general, people from lower socioeconomic groups are at greater risk of poor health, have higher rates of illness, disability and death, and live shorter lives than those from higher socioeconomic groups (AIHW 2016). People experiencing socioeconomic disadvantage are less likely to participate in screening programs, more likely to be obese, less likely to exercise and much more likely to smoke, which are all risk factors for cancer. In 2010–2014 age-standardised cancer incidence rates were higher in the lowest socioeconomic areas compared with the highest socioeconomic areas for all cancers combined (Cancer Australia 2019c).
Socioeconomic status and low health literacy are closely correlated. Therefore, effective communication with patients and carers is particularly important given the prevalence of low health literacy in Australia (estimated at 60 per cent of Australian adults) (ACSQHC 2014).
Consideration should be taken for cancer patients experiencing socioeconomic disadvantage to reduce their risk of being underserved for health care.
A diagnosis of cancer may present additional challenges to people who have pre-existing chronic mental health or psychiatric concerns, resulting in exacerbation of their mental health symptoms. This may include heightened anxiety, worsening depression or thoughts of self-harm.
As poor adjustment and coping can affect treatment decisions, people who are known to have a mental health diagnosis need psychosocial assessment in the oncology setting to formulate a plan for ongoing support throughout treatment.
Psychosocial support can assist with challenges in communicating with health professionals, enhance understanding of the treatment journey, ensure capacity for consent to treatment options and improve compliance with treatment requests. A referral for psychosocial support from a health professional to the psycho-oncology team can ensure these patients are provided with targeted interventions or referrals to community-based services that may mitigate problems associated with the impacts of social isolation that frequently accompany chronic mental ill-health.
Many patients with chronic mental health problems may be well known to external service providers. Psycho-oncology health professionals can form meaningful partnerships with existing service providers to optimise patient care throughout treatment and beyond.
Drug use disorders fall within the area of mental health conditions. People who are opiate dependent may have specific and individual requirements regarding pain management and their own preference for type of opiate prescribed or used.
People who identify as sexually or gender diverse may have unique needs following a cancer diagnosis. Sexually or gender diverse identities include (but are not limited to) people who identify as lesbian, gay, bisexual or transgender, collectively ‘LGBT’. There is no universally agreed upon initialism to describe this community, with other terms such as queer/questioning (Q), intersex (I), asexual (A) and pansexual (P) often included, as well as a plus symbol (+) indicating inclusivity of other identities not explicitly mentioned.
Sexual orientation and gender identity are relevant across the entire spectrum of cancer care, from prevention to survivorship and end-of-life care. LGBT people are less likely to participate in cancer screening, and some segments of the LGBT community exhibit elevated rates of specific cancer risk factors – for example, higher rates of smoking and alcohol use. Regarding treatment, there may be unique factors relevant to LGBT people that may affect decision making. Additionally, the LGBT population experiences higher rates of anxiety, depression and stressful life circumstances, and may be at risk of inferior psychosocial outcomes following a cancer diagnosis. LGBT people are also more likely to be estranged from their families of origin, and for older people, less likely to have adult children who may provide support and care.
Barriers to care for LGBT people include past negative interactions with healthcare systems, experiences or fear of discrimination and harassment in healthcare settings, assumptions of cisgender/heterosexual identity, lack of recognition or exclusion of same-sex partners from care, and a lack of relevant supportive care and information resources.
To provide safe and appropriate care for LGBT people with cancer, healthcare providers should:
- display environmental cues to show an inclusive and safe setting for LGBT patients
- avoid assumptions about the sexual orientation or gender identity of patients and their partners
- facilitate positive disclosure of sexual orientation or gender identity
- include same-sex/gender partners and families of choice in care
- be aware of relevant supportive care and information resources
- provide non-judgemental, patient-centred care
Supportive care in cancer refers to the following five domains:
- the physical domain, which includes a wide range of physical symptoms that may be acute, relatively short lived or ongoing, requiring continuing interventions or rehabilitation
- the psychological domain, which includes a range of issues related to the patient’s mental health wellbeing and personal relationships
- the social domain, which includes a range of social and practical issues that will affect the patient, carer and family such as the need for emotional support, maintaining social networks and financial concerns
- the information domain, which includes access to information about cancer and its treatment, recovery and survivorship support services and the health system overall
- the spiritual domain, which focuses on the patient’s changing sense of self and challenges to their underlying beliefs and existential concerns (Palliative Care Victoria 2019).
Fitch’s (2000) model of supportive care recognises the variety and level of intervention required at each critical point as well as the need to be specific to the individual patient. The model targets the type and level of intervention required to meet patients’ supportive care needs.
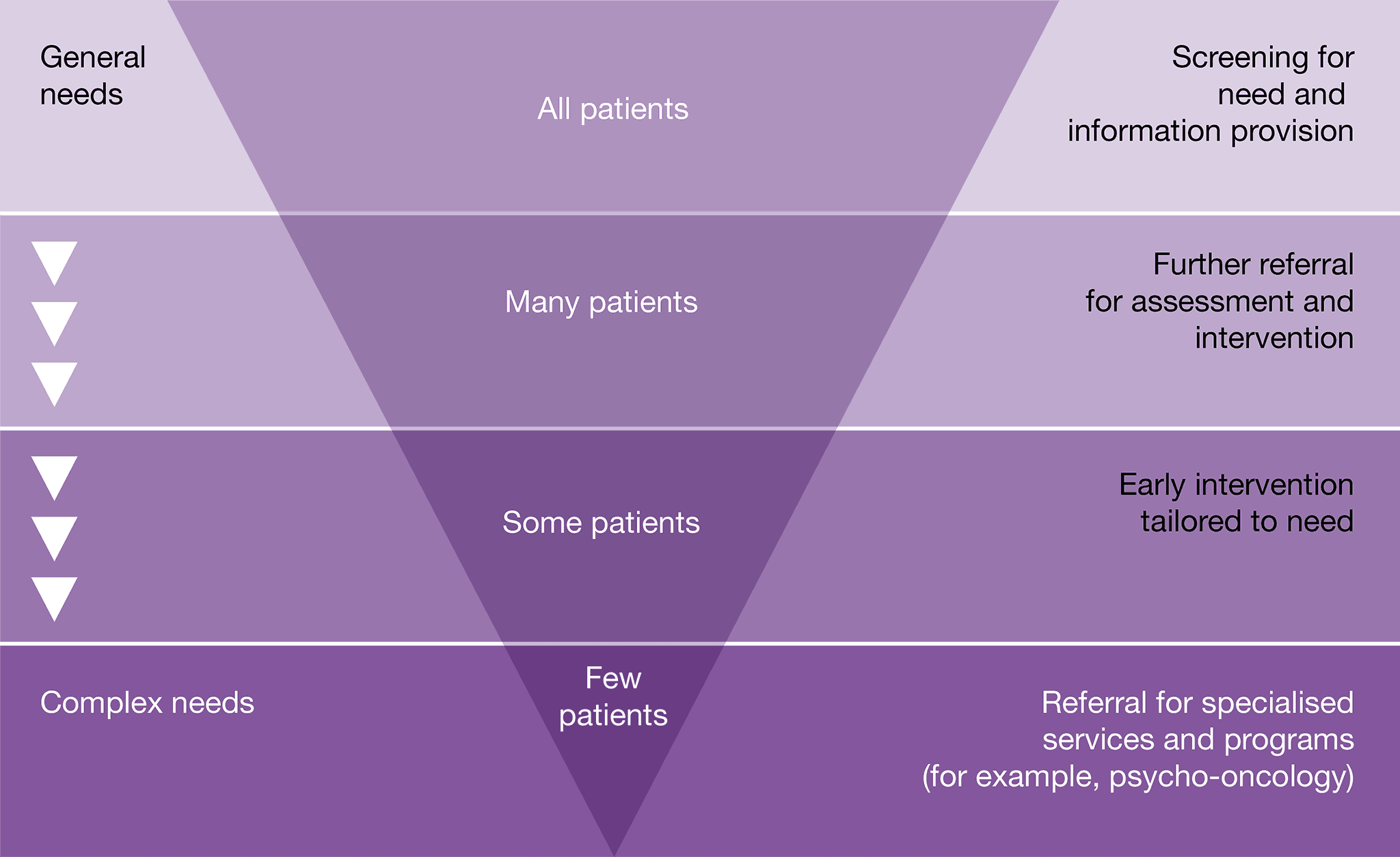
Consider a referral to a psychologist, psychiatrist, pastoral/spiritual care practitioner, social worker, specialist nurse or a relevant community-based program if the patient has these issues:
- displaying emotional cues such as tearfulness, distress that requires specialist intervention, avoidance or withdrawal
- being preoccupied with or dwelling on thoughts about cancer and death
- displaying fears about the treatment process or the changed goals of their treatment
- displaying excessive fears about cancer progression or recurrence
- worrying about loss associated with their daily function, dependence on others and loss of dignity
- becoming isolated from family and friends and withdrawing from company and activities that they previously enjoyed
- feeling hopeless and helpless about the effect that cancer is having on their life and the disruption to their life plans
- struggling to communicate with family and loved ones about the implications of their cancer diagnosis and treatment
- experiencing changes in sexual intimacy, libido and function
- struggling with the diagnosis of metastatic or advanced disease
- having difficulties quitting smoking (refer to Quitline on 13 7848) or with other drug and alcohol use
- having difficulties transitioning to palliative care.
Additional considerations that may arise for the multidisciplinary team include:
- support for the carer – encourage referrals to psychosocial support from a social worker, psychologist or general practitioner
- referral to an exercise physiologist or physiotherapist as a therapeutic approach to prevent and manage psychological health
- referral to wellness-after-cancer programs to provide support, information and offer strategies.
Complementary therapies may be used together with conventional medical treatments to support and enhance quality of life and wellbeing. They do not aim to cure the patient’s cancer. Instead, they are used to help control symptoms such as pain and fatigue (Cancer Council Australia 2019).
The lead clinician or health professional involved in the patient’s care should discuss the patient’s use (or intended use) of complementary therapies not prescribed by the multidisciplinary team to assess safety and efficacy and to identify any potential toxicity or drug interactions.
The lead clinician should seek a comprehensive list of all complementary and alternative medicines being taken and explore the patient’s reason for using these therapies and the evidence base. A transparent and honest discussion that is free from judgement should be encouraged.
While some complementary therapies are supported by strong evidence, others are not. For such therapies, the lead clinician should discuss their potential benefits and use them alongside conventional therapies (NHMRC 2014).
If the patient expresses an interest in using complementary therapies, the lead clinician should consider referring patients to health providers within the multidisciplinary team who have expertise in the field of complementary and alternative therapies (e.g. a clinical pharmacist, dietitian or psychologist) to assist them to reach an informed decision. Costs of such approaches should be part of the discussion with the patient and considered in the context of evidence of benefit.
The lead clinician should assure patients who use complementary therapies that they can still access a multidisciplinary team review and encourage full disclosure about therapies being used.
- See Cancer Australia’s position statement on complementary and alternative therapies
- See the Clinical Oncological Society of Australia’s position statement Use of complementary and alternative medicine by cancer patients
Advance Care Planning Australia
Advance Care Planning Australia provides national advance care planning resources for individuals, families, health professional and service providers. Resources include a national advisory service, information resources, a legal forms hub and education modules.
- Telephone: 1300 208 582
- Website
Australian Cancer Survivorship Centre
The Australian Cancer Survivorship Centre has developed information resources and events to help people move from initial treatment to post treatment and beyond, including those receiving maintenance treatments. While they do not provide clinical advice, they connect with a range of providers to enable improved care.
- Telephone: (03) 8559 6220
- Website
Australian Commission on Safety and Quality in Health Care
The Australian Commission on Safety and Quality in Health Care has developed a resource for patients and carers explaining the coordination of care that patients should receive from their health service during cancer treatment. The resource is called What to expect when receiving medication for cancer care.
Beyond Blue
Beyond Blue provides information about depression, anxiety and related disorders, as well as about available treatment and support services.
- Telephone: 1300 22 4636
- Website
Cancer Australia
Cancer Australia provides information for consumers, carers and their families including printed resources and video content.
Cancer Council’s Cancer Information and Support Service
Cancer Council 13 11 20 is a confidential telephone support service available to anyone affected by cancer. This service acts as a gateway to evidence-based documented, practical and emotional support available through Cancer Council services and other community organisations. Calls will be answered by a nurse or other oncology professional who can provide information relevant to a patient’s or carer’s situation. Health professionals can also access this service.
- Telephone: 13 11 20 – Monday to Friday, 9.00am to 5.00pm (some states have extended hours)
- Website
Cancer Council’s Cancer Connect
Cancer Connect is a free and confidential telephone peer support service that connects someone who has cancer with a specially trained volunteer who has had a similar cancer experience.
A Connect volunteer can listen with understanding and share their experiences and ways of coping. They can provide practical information, emotional support and hope. Many people newly diagnosed with cancer find this one-to-one support very beneficial.
For more information on Cancer Connect call Cancer Council on 13 11 20.
Canteen
Canteen helps adolescents, young adults and parents to cope with cancer in their family. Canteen offers individual support services, peer support services and a youth cancer service, as well as books, resources and useful links.
- Telephone: 1800 835 932 to talk to a health professional about information and support for young people or 1800 226 833 for other enquiries
- Website
Clinical trial information
For a collection of clinical trials available in Australia see the following sources of information:
CanEAT pathway
A guide to optimal cancer nutrition for people with cancer, carers and health professionals.
Guides to best cancer care
The short guides help patients, carers and families understand the optimal cancer care that should be provided at each step. They include optimal timeframes within which tests or procedures should be completed, prompt lists to support patients to understand what might happen at each step of their cancer journey and to consider what questions to ask, and provide information to help patients and carers communicate with health professionals.
The guides are located on an interactive web portal, with downloadable PDFs available in multiple languages.
Look Good, Feel Better
A free national community service program, run by the Cancer Patients Foundation, dedicated to teaching cancer patients how to manage the appearance-related side effects caused by treatment for any type of cancer.
- Telephone: 1800 650 960
- Website
National Comprehensive Cancer Network
The National Comprehensive Cancer Network’s Guideline for pancreatic cancer is based on the same treatment information doctors use and aim to help patients talk to their doctor about the best treatment options for them.
Pancare Foundation
A national non-for-profit organisation that aims to increase survival and supports patients with pancreatic and other gastrointestinal cancers.
- Phone: 1300 881 698
- Website
PanKind
A national organisation dedicated to doubling survival for pancreatic cancer patients through fundraising for research, advocacy, awareness and patient support.
- Phone: (02) 7207 6970
- Website
PanSupport
An online resource that focuses on patient care, advice on managing pancreatic cancer symptoms (such as with diet and fatigue) and activities that can strengthen mental health. There is information for carers and about organisations, support groups and tools that could assist patients.
Quitline
Quitline is a confidential, evidence-based telephone counselling service. Highly trained Quitline counsellors use behaviour change techniques and motivational interviewing over multiple calls to help people plan, make and sustain a quit attempt.
Quitline is a culturally inclusive service for all, and Aboriginal counsellors are also available. Health professionals can refer patients to Quitline online or via fax.
- Telephone: 13 7848
- Website or the relevant website in your state or territory.
Australian Cancer Survivorship Centre
The Australian Cancer Survivorship Centre provides expertise in survivorship care, information, support and education. Its purpose is to support and enable optimal survivorship care.
- Telephone: (03) 8559 6220
- Website
Australian Commission on Safety and Quality in Health Care
The Australian Commission on Safety and Quality in Health Care has developed a guide for clinicians containing evidence-based strategies to support clinicians to understand and fulfil their responsibilities to cancer patients. This guide is particularly relevant to steps 3 to 6 of the optimal care pathway. The guide is titled NSQHS Standards user guide for medication management in cancer care for clinicians.
Cancer Australia
Information for health providers including guidelines, cancer learnings, cancer guides, reports, resources, videos, posters and pamphlets.
Cancer Council Australia
Information on prevention, research, treatment and support provided by Australia’s peak independent cancer authority.
CanEAT pathway
A guide to optimal cancer nutrition for people with cancer, carers and health professionals.
Care Search: Palliative Care Knowledge Network
Information for patients and carers on living with illness, advice on how to care, and help finding services.
- Telephone: (08) 7221 8233
- Website
eviQ
A clinical information resource providing health professionals with current evidence-based, peer-maintained, best practice cancer treatment protocols and information relevant to the Australian clinical environment.
National Health and Medical Research Council
Information on clinical practice guidelines, cancer prevention and treatment.
Advance care directive – voluntary person-led document that focus on an individual’s values and preferences for future health and medical treatment decisions, preferred outcomes and care. They are completed and signed by a competent person. They are recognised by specific legislation (statutory) or common law (non-statutory). Advance care directives can also appoint the substitute decision-maker(s) who can make decisions about health or personal care on the individual’s behalf if they are no longer able to make decisions themselves. Advance care directives focus on the future health care of a person, not on the management of his or her assets. They come into effect when an individual loses decision-making capacity.
Advance care planning – the process of planning for future health and personal care, where the person’s values, beliefs and preferences are made known so they can guide decision making at a future time when that person cannot make or communicate their decisions.
Alternative therapies – treatments used in place of conventional medical treatment.
Care coordinator – the health provider nominated by the multidisciplinary team to coordinate patient care. The care coordinator may change over time depending on the patient’s stage in the care pathway and the location and care in which care is being delivered.
Castrate resistant progressive disease – progressive disease despite castrate levels of testosterone (Cancer Council Australia Advanced Prostate Cancer Guidelines Working Party 2010).
Complementary therapies – supportive treatment used in conjunction with conventional medical treatment. These treatments may improve wellbeing and quality of life and help people deal with the side effects of cancer.
End-of-life care – includes physical, spiritual and psychosocial assessment, and care and treatment, delivered by health professionals and ancillary staff. It also includes support of families and carers and care of the patient’s body after their death.
Immunotherapy – a type of cancer treatment that helps the body’s immune system to fight cancer. Immunotherapy can boost the immune system to work better against cancer or remove barriers to the immune system attacking the cancer.
Indicator – a documentable or measurable piece of information regarding a recommendation in the optimal care pathway.
Informed financial consent – the provision of cost information to patients, including notification of likely out-of-pocket expenses (gaps), by all relevant service providers, preferably in writing, before admission to hospital or treatment (Commonwealth Department of Health 2017).
Lead clinician – the clinician who is nominated as being responsible for individual patient care. The lead clinician may change over time depending on the stage of the care pathway and where care is being provided.
Metastatic disease – cancer that has spread from the part of the body where it started (the primary site) to other parts of the body.
Multidisciplinary care – an integrated team approach to health care in which medical and allied health providers consider all relevant treatment options and collaboratively develop an individual treatment plan for each patient.
Multidisciplinary team – comprises the core disciplines that are integral to providing good care. The team is flexible in approach, reflects the patient’s clinical and psychosocial needs and has processes to facilitate good communication.
Multidisciplinary team meeting – a meeting of health professionals from one or more clinical disciplines who together make decisions about recommended treatment of patients.
Optimal care pathway – the key principles and practices required at each stage of the care pathway to guide the delivery of consistent, safe, high-quality and evidence-based care for all people affected by cancer.
Palliative care – any form of medical care or treatment that concentrates on reducing the severity of disease symptoms.
Patient management frameworks – tumour stream models adopted in Victoria in 2003 to reduce variation in cancer care. The optimal care pathways are updated versions of these models.
Performance status – an objective measure of how well a patient can carry out activities of daily life.
Prehabilitation – one or more interventions performed in a newly diagnosed cancer patient that are designed to improve physical and mental health outcomes as the patient undergoes treatment and beyond.
Primary care health professional – in most cases this is a general practitioner but may also include general practice nurses, community nurses, nurse practitioners, allied health professionals, midwives, pharmacists, dentists and Aboriginal health workers.
Primary specialist – the person who makes the referral to the multidisciplinary team (such as specialist physician, surgeon, oncologist, palliative care specialist). This person will also make referrals for treatment and will be responsible for overseeing follow-up care.
PSMA PET/CT – a whole body scan that images prostate cancer wherever it is located in the body.
Rehabilitation – comprises multidisciplinary efforts to allow the patient to achieve optimal physical, social, physiological and vocational functioning within the limits imposed by the disease and its treatment.
Spiritual care – the aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred.
Substitute decision-maker – a person permitted under the law to make decisions on behalf of someone who does not have competence or capacity.
Supportive care – care and support that aims to improve the quality of life of people living with cancer, cancer survivors and their family and carers and particular forms of care that supplement clinical treatment modalities.
Survivorship – an individual is considered a cancer survivor from the time of diagnosis, and throughout their life; the term includes individuals receiving initial or maintenance treatment, in recovery or in the post-treatment phase.
Survivorship care plan – a formal, written document that provides details of a person’s cancer diagnosis and treatment, potential late and long-term effects arising from the cancer and its treatment, recommended follow-up, surveillance, and strategies to remain well.
Targeted therapy – a medicine that blocks the growth and spread of cancer by interfering with specific molecules.
We acknowledge the Traditional Owners of Country throughout Australia and their continuing connection to the land, sea and community. We pay our respects to them and their cultures and to Elders past, present and emerging.
This work is available from the Cancer Council website.
First published in May 2015. This edition published in June 2021.
ISBN: 978 1 76096 157 2
Cancer Council Victoria and Department of Health Victoria 2021 Optimal care pathway for people with pancreatic cancer, 2nd edn, Cancer Council Victoria, Melbourne.
Enquiries about this publication can be sent to optimalcare.pathways@cancervic.org.au.
Our thanks to the following health professionals, consumer representatives, stakeholders and organisations consulted in developing this optimal care pathway.
Professor Christopher Christophi (Chair), Surgeon, Austin Health and The University of Melbourne
Dr Richard Khor, Radiation Oncologist, Austin Health and Olivia Newton-John Cancer Centre
Professor Michael Michael, Medical Oncologist, Peter MacCallum Cancer Centre
Dr Krithika Murali, Clinical Geneticist Fellow, Victorian Clinical Genetics Services
Dr Mehrdad Nikfarjam, Surgeon, Austin Health
Ms Rose Rocca, Dietitian, Peter MacCallum Cancer Centre
Mr Jim Siderov, Pharmacist, Austin Health
Associate Professor Odette Spruijt, Palliative Care Consultant, Peter MacCallum Cancer Centre
Professor Robert Thomas, Special Advisor on Health, Professorial Fellow, The University of Melbourne
Ms Julia Brancato, Project Coordinator, Optimal Care Pathways, Cancer Council Victoria
Professor Chris Christophi, The University of Melbourne, Department of Surgery, Austin Health (Chair)
Professor Jon Emery, Herman Professor of Primary Care, The University of Melbourne, Western Health; Director of Primary Care Collaborative Cancer Trials Group
Mr Adrian Fox, Hepatobiliary Surgeon, Eastern Health
Associate Professor Sze Ting Lee, Nuclear Medicine Physician, Centre for PET, Austin Health
Ms Helen Mott, Cancer Support Nurse, Haematology Oncology, Alfred Health
Associate Professor Vijayaragavan Muralidharan, Hepatobiliary Surgeon, The University of Melbourne, Austin Health
Dr Mehrdad Nikfarjam, Pancreas Surgeon, The University of Melbourne, Austin Health
Ms Lucy Pollerd, Social Worker, Peter MacCallum Cancer Centre
Ms Meg Rogers, Nurse Coordinator, Upper Gastrointestinal Cancer Service, Peter MacCallum Cancer Centre
Ms Amy Sutherland, Dietitian, Northern Health
Professor Robert Thomas, Chief Cancer Advisor, Department of Health and Human Services
Ms Kathryn Whitfield, Acting Manager, Cancer Strategy and Development, Department of Health and Human Services
Alexandra Viner, Project Manager –Optimal Care Pathways
Advance Care Planning Australia
Allied Health Professions Australia
Australasian Association of Nuclear Medicine Specialists
Australasian Chapter of Palliative Medicine, Royal Australia College of Physicians
Australasian Pancreatic Club
Australia and New Zealand Hepatic, Pancreatic and Biliary Association
Australian and New Zealand Gastric and Oesophageal Surgery Association
Australian and New Zealand Society of Neuroradiology
Australian and New Zealand Society of Palliative Care
Australian Cancer Survivorship Centre
Australian College of Nursing
Australian Medical Association
Australian Society of Medical Imaging and Radiation Therapy
PanKind
Cancer Nurses Society of Australia
Clinical Oncology Society of Australia
Interventional Radiology Society of Australasia
Medical Oncology Group of Australia
Oncology Social Workers Australia and New Zealand
Royal Australasian College of Physicians
Royal Australasian College of Surgeons
Royal Australian and New Zealand College of Radiologists
Royal Australian College of General Practitioners
Royal College of Pathologists of Australasia
Upper Gastrointestinal Cancer Registry
Alfred Health
Cancer Australia
Cancer Council Victoria, Strategy and Support Division
Cancer Institute New South Wales
Concord Repatriation General Hospital New South Wales
Consumer representative
Department of Health Victoria, Commissioning and System Improvement Division, Cancer Unit
National Cancer Expert Reference Group
Olivia Newton-John Cancer Wellness and Research Centre
St Vincent’s Hospital Melbourne
Other stakeholders consulted to provide feedback include relevant Cancer Council committees and networks, Integrated Cancer Services, Primary Health Networks and several health services.
The multidisciplinary team may include the following members:
- care coordinator (as determined by multidisciplinary team members)*
- dietitian*
- gastroenterologist (with expertise in endoscopic retrograde cholangiopancreatography (ERCP) and/or endoscopic ultrasound)*
- hepato-pancreato biliary surgeon*
- interventional/ hepato-pancreato biliary radiologist*
- nurse (with appropriate expertise)*
- medical oncologist*
- radiation oncologist*
- palliative care specialist*
- pathologist*
- Aboriginal health practitioner, Indigenous liaison officer or remote general practitioner
- clinical trials coordinator
- exercise physiologist
- fertility specialist
- general practitioner
- nuclear medicine physician
- occupational therapist
- pharmacist
- physiotherapist
- psychiatrist
- psychologist
- social worker
- spiritual/pastoral care.
* Denotes core members. Core members of the multidisciplinary team are expected to attend most multidisciplinary team meetings either in person or remotely.
Amanam I, Chung V 2018, ‘Target therapies for pancreatic cancer’, Cancers, vol. 10, no. 2, p. 36.
American Cancer Society 2019, ‘Pancreatic cancer’, viewed 12 December 2019, http://www.cancer.org/cancer/pancreatic-cancer/causes-risks-prevention/prevention.html.
American Society of Clinical Oncology (ASCO) 2019, Maintenance therapy with PARP inhibitor olaparib delays progression of BRCA-related pancreatic cancer, news release, viewed 27 January 2021, https://www.asco.org/about-asco/press-center/news-releases/maintenance-therapy-parp-inhibitor-olaparib-delays-progression.
Arriaga ME, Vajdic CM, MacInnis RJ, Canfell K, Magliano DJ, Shaw JE, et al. 2019, ‘The burden of pancreatic cancer in Australia attributable to smoking’, Medical Journal of Australia, vol. 210, no. 5, pp. 213–220.
Australian Adult Cancer Pain Management Guideline Working Party 2019, Australian adult cancer pain management guideline: ‘Cancer pain management in adults’, Cancer Council Australia, Sydney, viewed 6 June 2019, https://wiki.cancer.org.au/australiawiki/index.php?oldid=191646.
Australian Cancer Survivorship Centre 2016, ‘Survivorship care planning’, viewed 2 October 2020, https://www.petermac.org/sites/default/files/page/downloads/Survivorship_Care_Planning.pdf.
Australian Cancer Survivorship Centre 2019, Community support organisations’ cancer survivorship care consensus statement, viewed 10 February 2020, https://www.petermac.org/sites/default/files/media-uploads/NGO_ConsensusStatement.pdf.
Australian Clinical Trials 2015, ‘Potential benefits and risks’, National Health and Medical Research Council, Department of Industry, Innovation and Science, Australian Government, Canberra, viewed 24 July 2019, https://www.australianclinicaltrials.gov.au/why-be-part-clinical-trial/potential-benefits-and-potential-risks.
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2014, Health literacy: taking action to improve safety and quality, ACSQHC, Sydney, viewed 18 February 2020, https://www.safetyandquality.gov.au/sites/default/files/migrated/Health-Literacy-Taking-action-to-improve-safety-and-quality.pdf.
Australian Commission for Safety and Quality in Health Care (ACSQHC) 2015, Credentialing health practitioners and defining their scope of clinical practice: a guide for managers and practitioners, ACSQHC, Sydney, viewed 18 February 2020, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/credentialing-health-practitioners-and-defining-their-scope-clinical-practice-guide-managers-and-practitioners.
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2017, National Safety and Quality Health Service Standards guide for hospitals, ACSQHC, Sydney, viewed 18 February 2020, https://www.safetyandquality.gov.au/wp-content/uploads/2017/12/National-Safety-and-Quality-Health-Service-Standards-Guide-for-Hospitals.pdf.
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2019a, Person-centred care, ACSQHC, Sydney, viewed 15 May 2020, https://www.safetyandquality.gov.au/our-work/partnering-consumers/person-centred-care.
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2019b, Australian Hospital Patient Experience Question Set, ACSQHC, Sydney, viewed 25 March 2020, https://www.safetyandquality.gov.au/our-work/indicators-measurement-and-reporting/australian-hospital-patient-experience-question-set.
Australian Commission for Safety and Quality in Health Care (ACSQHC) 2020, ‘NSQHS Standards user guide for medication management in cancer care’, ACSQHC, Sydney, viewed 16 April 2020, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/nsqhs-standards-user-guide-medication-management-cancer-care.
Australian Health Ministers’ Advisory Council (AHMAC) 2011, A national framework for advance care directives, Council of Australian Governments Health Council, Adelaide, viewed 22 July 2019, http://www.coaghealthcouncil.gov.au/Portals/0/A%20National%20Framework%20for%20Advance%20Care%20Directives_September%202011.pdf.
Australian Institute of Health and Welfare (AIHW) 2016, Australia’s health 2016, Australia’s health series no. 15. Cat. no. AUS 199, AIHW, Canberra.
Australia Institute of Health and Welfare (AIHW) 2017a, Cancer in Australia 2017, viewed 19 November 2020, https://www.aihw.gov.au/reports/cancer/cancer-in-australia-2017/contents/summary.
Australian Institute of Health and Welfare (AIHW) 2017b, Access to health services by Australians with disability, viewed 20 February 2020, https://www.aihw.gov.au/reports/disability/access-health-services-disability/contents/content.
Australian Institute of Health and Welfare (AIHW) 2018, Australia’s health 2018, Australia’s health series no. 16. Cat. no. AUS 221, AIHW, Canberra.
AYA Cancer Fertility Preservation Guidance Working Group 2014, Fertility preservation for AYAs diagnosed with cancer: guidance for health professionals, Cancer Council Australia, Sydney, viewed 20 July 2020, https://wiki.cancer.org.au/australia/COSA:AYA_cancer_fertility_preservation/Introduction.
Cancer Australia 2015, National Aboriginal and Torres Strait Islander cancer framework, Cancer Australia, Surry Hills, viewed 24 August 2017, https://www.canceraustralia.gov.au/publications-and-resources/cancer-australia-publications/national-aboriginal-and-torres-strait-islander-cancer-framework.
Cancer Australia 2017a, Pancreatic cancer, viewed 11 December 2019, https://pancreatic-cancer.canceraustralia.gov.au/home.
Cancer Australia 2017b, Principles of cancer survivorship, Australian Government, Sydney, viewed 18 February 2020, https://canceraustralia.gov.au/sites/default/files/publications/principles-cancer-survivorship/pdf/pocs_-_principles_of_cancer_survivorship.pdf.
Cancer Australia 2019a, Principles of multidisciplinary care, Australian Government, Sydney, viewed 18 July 2019, https://canceraustralia.gov.au/system/tdf/guidelines/all_about_multidisciplinary_care.pdf?file=1&type=node&id=3551.
Cancer Australia 2019b, National Cancer Control Indicators: Pancreatic cancer, viewed 12 December 2019, https://ncci.canceraustralia.gov.au/cancer-types/pancreatic-cancer.
Cancer Australia 2019c, ‘Cancer incidence’, viewed 18 February 2020, https://ncci.canceraustralia.gov.au/diagnosis/cancer-incidence/cancer-incidence.
Cancer Australia 2020a, Cancer care in the time of COVID-19: a conceptual framework for the management of cancer during a pandemic, Australian Government, Sydney, viewed 3 September 2020, https://www.canceraustralia.gov.au/publications-and-resources/cancer-australia-publications/cancer-care-time-covid-19-conceptual-framework-management-cancer-during-pandemic.
Cancer Australia 2020b, Pancreatic cancer in Australia statistics, viewed 19 November 2020, https://www.canceraustralia.gov.au/affected-cancer/cancer-types/pancreatic-cancer/statistics.
Cancer Council Australia 2018, ‘Prevention’, Cancer Council Australia, Sydney, viewed 18 July 2019, https://www.cancer.org.au/preventing-cancer/.
Cancer Council Australia 2019, ‘Complementary and alternative therapies’, Cancer Council Australia, Sydney, viewed 22 July 2019, https://www.cancer.org.au/about-cancer/treatment/complementary-therapies-and-cancer.html.
Cancer Council Victoria 2019, ‘Palliative care’, Cancer Council Victoria, viewed 7 October 2019, https://www.cancervic.org.au/cancer-information/treatments/treatments-types/palliative_care/palliative-care-treatment.html.
Cancer Research in Primary Care 2016, Principles statement: Shared care, PC4 Shared Care Working Group, Melbourne, viewed 4 October 2019, http://pc4tg.com.au/wp-content/uploads/2016/07/PC4-Principles-Statement-shared-care-2016-1.pdf.
Clinical Oncology Society of Australia (COSA) 2013, Special Issue: COSA’s 40th Annual Scientific Meeting, Cancer Care Coming of Age, 12–14 November 2013, Adelaide Convention Centre, Asia-Pacific Journal of Clinical Oncology, vol. 9, no. 3, pp. 61–98.
Clinical Oncology Society of Australia (COSA) 2014, Psychosocial management of AYAs diagnosed with cancer: guidance for health professionals, COSA, Sydney, viewed 7 October 2019, http://wiki.cancer.org.au/australia/COSA:Psychosocial_management_of_AYA_cancer_patients.
Clinical Oncology Society of Australia (COSA) 2015, Cancer care coordinator: position statement, COSA, Sydney, viewed 22 July 2019, https://www.cosa.org.au/media/332296/cancer-care-coordinator-position-statement_final-endorsed-by-council_161115_cnsa-logo.pdf.
Clinical Oncology Society of Australia (COSA) 2016, Australasian tele-trial model: access to clinical trials closer to home using tele-health a national guide for implementation, v1.7, COSA, Sydney, viewed 18 July 2019, https://www.cosa.org.au/media/332325/cosa-teletrial-model-final-19sep16.pdf.
Clinical Oncology Society of Australia (COSA) 2018, COSA position statement on exercise in cancer care, COSA, Sydney, viewed 22 July 2019, https://www.cosa.org.au/media/332488/cosa-position-statement-v4-web-final.pdf.
Commonwealth Department of Health 2017, Out-of-pocket expenses for private medical treatment (informed financial consent), Commonwealth of Australia, Canberra.
Cormie P, Atkinson M, Bucci L, Cust A, Eakin E, Hayes S, et al. 2018, ‘Clinical Oncology Society of Australia position statement on exercise in cancer care’, Medical Journal of Australia, vol. 209, no. 4, pp. 184–187.
Cormie P, Zopf EM, Zhang X, Schmitz KH 2017, ‘The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects’, Epidemiologic Reviews, vol. 39, no. 1, pp. 71–92.
Decoster L, Van Puyvelde K, Mohile S, Wedding U, Basso U, Colloca G, et al. 2015, ‘Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendations’, Annals of Oncology, vol. 26, no.1, pp. 288–300.
Emery J 2014, ‘Cancer survivorship – the role of the GP’, Australian Family Physician, vol. 43, no. 8, pp. 521–525.
Elbanna KY, Jang H, Kim TK 2020, ‘Imaging diagnosis and staging of pancreatic ductal adenocarcinoma: a comprehensive review’, Insights Imaging, vol. 11, no. 58, doi: 10.1186/s13244-020-00861-y.
eviQ 2019, ‘Safe handling and waste management of hazardous drugs’, Cancer Institute NSW, Sydney, viewed 22 July 2019, https://www.eviq.org.au/clinical-resources/administration-of-antineoplastic-drugs/188-safe-handling-and-waste-management-of-hazardou.
Ferrari A, Thomas D, Franklin A, Hayes-Lattin B, Mascarin M, van der Graaf W, et al. 2010, ‘Starting an adolescent and young adult program: some success stories and some obstacles to overcome’, Journal of Clinical Oncology, vol. 28, no. 32, pp. 4850–4857.
Fitch M 2000, ‘Supportive care for cancer patients’, Hospital Quarterly, vol. 3, no. 4, pp. 39–46.
Fitch MI 2008, ‘Supportive care framework’, Canadian Oncology Nursing Journal, vol. 18, no. 1, pp. 6–14.
Freelove R, Walling A 2006, ‘Pancreatic cancer: diagnosis and management’, American Family Physician, vol. 73, no. 3, pp. 485–492.
Gaertner J, Wolf J, Hallek M, Glossmann JP, Voltz R 2011, ‘Standardizing integration of palliative care into comprehensive cancer therapy – a disease specific approach’, Supportive Care in Cancer’, vol. 19, no. 7, pp. 1037–1043.
Gilligan T, Coyle N, Frankel RM, Berry DL, Bohlke K, Epstein, RM, et al. 2017, ‘Patient–clinician communication: American Society of Clinical Oncology consensus guideline’, Journal of Clinical Oncology, vol. 35, no. 31, pp. 3618–3623.
Goggins M, Overbeek KA, Brand R, Syngal S, Del Chiaro M, Bartsch DK, et al. 2019, ‘Management of patients with increased risk for familial pancreatic cancer: updated recommendations from the International Cancer of the Pancreas Screening (CAPS) Consortium’, British Medical Journal, vol. 69, pp. 7–17.
Hack TF, Reuther DJ, Weir LM, Grenier D, Degner LF 2012, ‘Promoting consultation recording practice in oncology: identification of critical implementation factors and determination of patient benefit’, Psycho-Oncology, vol. 22, pp. 1273–1282.
Haines IE 2011, ‘Managing patients with advanced cancer: the benefits of early referral for palliative care’, Medical Journal of Australia, vol. 194, no. 3, pp. 107–108.
Hata T, Motoi F, Masahau I, Naitoh T, Katayose Y, Egawa S, et al. 2016, ‘Effect of hospital volume on surgical outcomes after pancreaticoduodenectomy’, Annals of Surgery, vol. 263, no. 4, pp. 334–672.
Hayes SC, Newton RU, Spence RR, Galvao DA 2019, ‘The Exercise and Sports Science Australia position statement: exercise medicine in cancer management’, Journal of Science and Medicine in Sport, vol. 22, no. 11, pp. 1175–1199.
Hewitt M, Greenfield S, Stovall E 2006, From cancer patient to cancer survivor: lost in transition, National Academies Press, Washington.
Jefford M, Ward AC, Lisy K, Lacey K, Emery JD, Glaser AW, et al. 2017, ‘Patient-reported outcomes in cancer survivors: a population-wide cross-sectional study’, Support Care Cancer, no. 10, pp. 3171–3179.
Kamisawa T, Wood LD, Itoi T, Takaori K 2016, ‘Pancreatic cancer’, Lancet, vol. 388, no. 10039, pp. 73–85.
Laidsaar-Powell R, Butow P, Boyle F, Juraskova 2018a, ‘Facilitating collaborative and effective family involvement in the cancer setting: guidelines for clinicians (TRIO guidelines-1)’, Patient Education and Counseling, vol. 101, no. 6, pp. 970–982.
Laidsaar-Powell R, Butow P, Boyle F, Juraskova 2018b, ‘Managing challenging interactions with family caregivers in the cancer setting: guidelines for clinicians (TRIO guidelines-2)’, Patient Education and Counselling, vol. 101, no. 6, pp. 983–994.
Lambert A, Schwarz L, Borbath I, Henry A, Laetham JV, Malka D, et al. 2019, ‘An update on treatment options for pancreatic adenocarcinoma’, Therapeutic Advances in Medical Oncology, vol. 11, pp. 1–43.
Lei Q, Zheng H, Bi J, Wang X, Jiang T, Gao X, et al. 2016, ‘Whole grain intake reduces pancreatic cancer risk: a meta-analysis of observational studies’, Medicine, vol. 95, no. 9, e.2747.
Loeliger J, Dewar S 2019, The CanEAT pathway for health professionals: a guide to optimal cancer nutrition care, Victorian Cancer Malnutrition Collaborative, Melbourne, viewed 22 June 2020, https://www.petermac.org/sites/default/files/media-uploads/Health%20professional%20pathway_231219_2.pdf.
Lisy K, Langdon L, Piper A, Jefford M 2019, ‘Identifying the most prevalent unmet needs of cancer survivors in Australia: a systematic review’, Asia-Pacific Journal of Clinical Oncology, vol. 15, no. 5, pp. e68–e78.
Monterosso L, Platt V, Bulsara M, Berg M 2019, ‘Systematic review and meta-analysis of patient reported outcomes for nurse-led models of survivorship care for adult cancer patients’, Cancer Treatment Reviews Journal, no. 73, pp. 62–72.
My Health Record 2019, ‘What is My Health Record?’ Australian Government, Sydney, viewed 17 December 2019, https://www.myhealthrecord.gov.au/for-you-your-family/what-is-my-health-record.
National Cancer Institute (NCI) 2019a, Pancreatic cancer treatment (adult) (PDQ) – health professional version, viewed 12 December 2019, https://www.cancer.gov/types/pancreatic/hp/pancreatic-treatment-pdq#section/all.
National Cancer Institute (NCI) 2019b, Unusual cancers of childhood treatment (PDQ) – health professional version, viewed 13 December 2019, https://www.cancer.gov/types/childhood-cancers/hp/unusual-cancers-childhood-pdq#_sm_CDR0000799716_2185_toc.
National Cancer Survivorship Initiative (NCSI) 2015, ‘Stratified pathways of care’, National Health Service, UK, viewed 2 March 2015.
National Disability Insurance Agency 2018, ‘How the NDIS works’, NDIS, Canberra, viewed 3 June 2019, https://www.ndis.gov.au/understanding/how-ndis-works.
National Health and Medical Research Council (NHMRC) 2013, Personalised medicine and genetics, viewed 3 June 2019, https://www.nhmrc.gov.au/about-us/publications/personalised-medicine-and-genetics.
National Health and Medical Research Council (NHMRC) 2014, Talking with your patients about complementary medicine: a resource for clinicians, NHMRC, Canberra, viewed 18 February 2020, https://www.caresearch.com.au/caresearch/ClinicalPractice/PatientConsiderations/ComplementaryTherapies/tabid/1258/Default.aspx.
National Institute for Health and Care Excellence (NICE) 2015, Suspected cancer: recognition and referral, NICE Guidelines: National Institute for Health and Care Excellence. Published June 2015, viewed November 2019, https://www.nice.org.uk/guidance/ng12/chapter/1-Recommendations-organised-by-site-of-cancer.
palliAGED 2018, ‘Needs Assessment’, Flinders University, Bedford Park, viewed 1 October 2019, https://www.palliaged.com.au/tabid/4879/Default.aspx.
Palliative Care Australia 2018, National Palliative Care Standards, 5th edn, Palliative Care Australia, Canberra, viewed 24 July 2019, http://palliativecare.org.au/wp-content/uploads/dlm_uploads/2018/11/PalliativeCare-National-Standards-2018_Nov-web.pdf.
Palliative Care Victoria 2019, ‘Spiritual care’, Palliative Care Victoria, Melbourne, viewed 22 July 2019, https://www.pallcarevic.asn.au/healthcare-professionals/about-palliative-care/care/spiritual-care/.
Pericleous M, Rossi RE, Mandair D, Whyand T, Caplin ME 2014 ‘Nutrition and pancreatic cancer: anticancer research’, International Journal of Cancer Research Treatment, no. 34, pp. 9–22.
Peter MacCallum Cancer Centre 2019, Community support organisations’ cancer survivorship care consensus statement, viewed 10 February 2020, https://www.petermac.org/sites/default/files/media-uploads/NGO_ConsensusStatement.pdf.
Pietryga JA, Morgan DE 2015, ‘Imaging preoperatively for pancreatic adenocarcinoma’, Journal of Gastrointestinal Oncology, vol. 6, no. 4, pp. 343–357.
Queensland Health 2015, Sad news sorry business: guidelines for caring for Aboriginal and Torres Strait Islander people through death and dying, State Government of Queensland, Brisbane, viewed 22 July 2019, https://www.health.qld.gov.au/__data/assets/pdf_file/0023/151736/sorry_business.pdf.
Silver JK, Baima J 2013, ‘Cancer prehabilitation: an opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes’, American Journal of Physical Medicine & Rehabilitation, vol. 92, no. 8, pp. 715–727.
Silver JK 2015, ‘Cancer prehabilitation and its role in improving health outcomes and reducing health care costs’, Seminars in Oncology Nursing, vol. 31, no. 1, pp. 1–3.
Sjoquist K, Zalcberg J 2013, ‘Clinical trials – advancing cancer care’, Cancer Forum, vol. 37, no. 1, pp. 80–88.
Smith A, Bellizzi K, Keegan T, Zebrack B, Chen V, Neale A, et al. 2013, ‘Health-related quality of life of adolescent and young adult patients with cancer in the United States: the Adolescent and Young Adult Health Outcomes and Patient Experience Study’, Journal of Clinical Oncology, vol. 31, no. 17, pp. 2136–2145.
Smith S, Case L, Waterhouse K, Pettitt N, Beddard L, Oldham J, et al. 2012, A blueprint of care for teenagers and young adults with cancer, Teenage Cancer Trust, Manchester, UK.
Steer B, Marx G, Singhal N, McJannett M, Goldstein D, Prowse R 2009, ‘Cancer in older people: a tale of two disciplines’, Internal Medicine Journal, vol. 39, pp. 771–775.
Tan SY, Turner J, Kerin-Ayres K, Butler S, Deguchi C, Khatri S, et al. 2019, ‘Health concerns of cancer survivors after primary anti-cancer treatment’, Support Cancer Care, no. 10, pp. 3739–3747.
Temel J, Greer J, Muzikansky A, Gallagher E, Admane S, Jackson V 2010, ‘Early palliative care for patients with non-metastatic non-small cell lung cancer’, New England Journal of Medicine, vol. 363, no. 8, pp. 733–742.
Toomey PG, Teta AF, Patel KD, Ross SB, Rosemurgy AS 2016, ‘High-volume surgeons vs high-volume hospitals: are best outcomes more due to who or where?’, The American Journal of Surgery, vol. 211, no. 1, pp. 59–63.
Vardy JL, Raymond JC, Koczwara B, Lisy K, Cohn RJ, Joske D, et al. 2019, ‘Clinical Oncology Society of Australia position statement on cancer survivorship care’, Australian Journal of General Practice, vol. 48, no.12, pp. 833–836.
Vijayvergia N, Denlinger CS 2015, ‘Lifestyle factors in cancer survivorship: where we are and where we are headed’, Journal of Personalized Medicine, vol. 5, no. 3, pp. 243–263.
Wildiers H, Heeren P, Puts M, Topinkova E, Maryska LG, Janssen-Heijnen MLG, et al. 2014, ‘International Society of Geriatric Oncology Consensus on geriatric assessment in older patients with cancer’, Journal of Clinical Oncology, vol. 32, no. 24, pp. 2595–2603.
World Health Organization (WHO) 2018, ‘Malnutrition’, WHO, Geneva, viewed 18 July 2019, https://www.who.int/news-room/fact-sheets/detail/malnutrition.
Xu M, Jung X, Hines OJ, Eibl G, Chen Y 2018, ‘Obesity and pancreatic cancer: overview of epidemiology and potential prevention by weight loss’, Pancreas, vol. 47, no. 2, pp. 158–162.
Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, et al. 2014, ‘Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial’, Lancet, vol. 383, no. 9930, pp. 1721–1730.







