Blood Cancer – Low-Grade Lymphomas
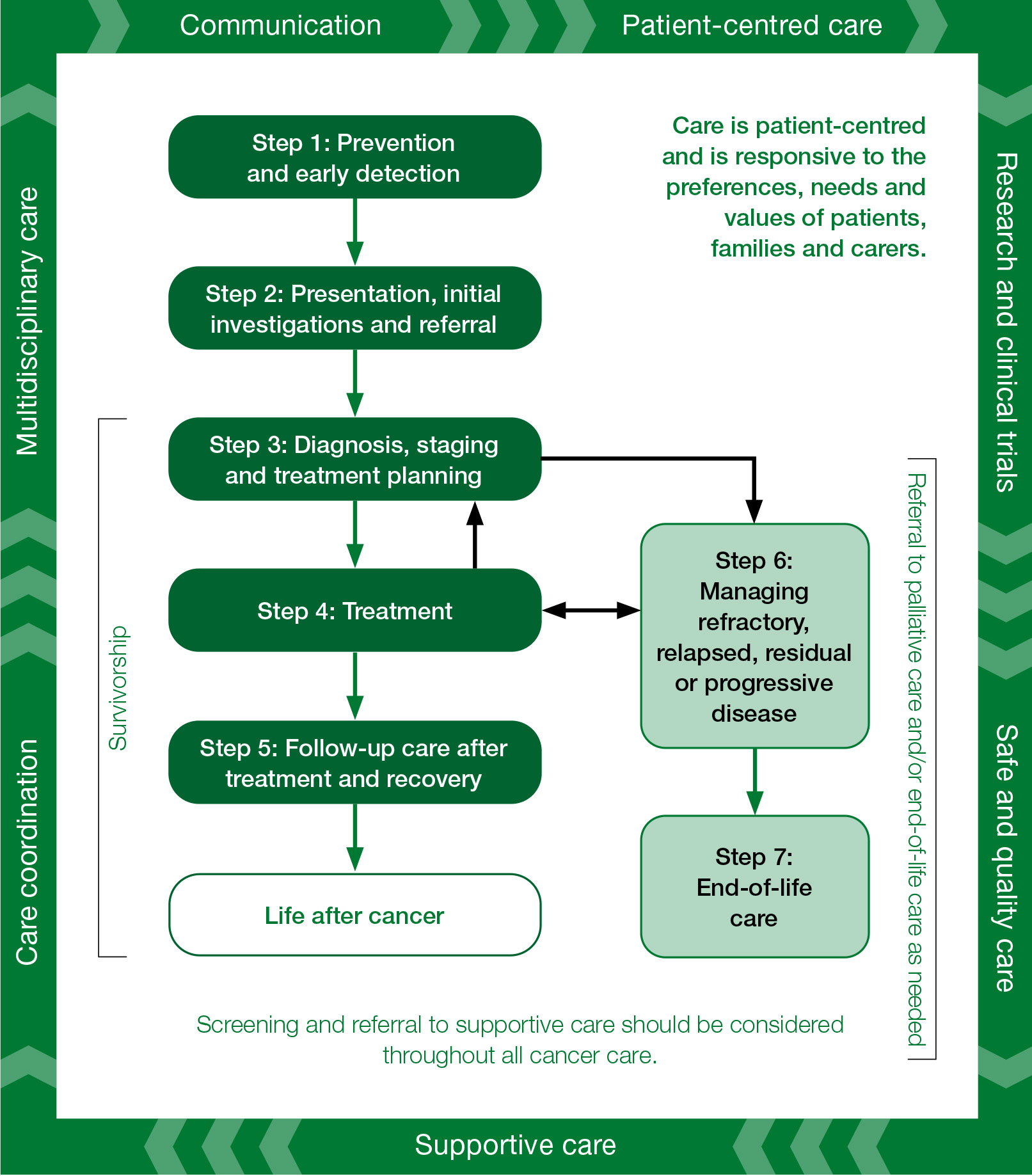
Optimal care pathways map seven key steps in cancer care. Each of these steps outlines nationally agreed best practice for the best level of care. While the seven steps appear in a linear model, in practice, patient care does not always occur in this way but depends on the particular situation (e.g. the type of cancer, the age of the patient, when and how the cancer is diagnosed, prognosis, management, the patients and carers decisions and their physiological response to treatment).
The principles underpinning optimal care pathways always put patients at the centre of care throughout their experience and prompt the healthcare system to deliver coordinated care.
The optimal care pathways do not constitute medical advice or replace clinical judgement, and they refer to clinical guidelines and other resources where appropriate.
Evidence-based guidelines, where they exist, should inform timeframes. Treatment teams need to recognise that shorter timeframes for appropriate consultations and treatment can promote a better experience for patients. Three steps in the pathway specify timeframes for care (Figure 3). They are designed to help patients understand the timeframes in which they can expect to be assessed and treated, and to help health services plan care delivery in accordance with expert-informed time parameters to meet the expectation of patients. These timeframes are based on expert advice from the Low-Grade Lymphomas Working Group.
Timeframes for care
| Step in pathway | Care point | Timeframe |
| Presentation, initial investigations and referral | Signs and symptoms | Presenting symptoms should be promptly and clinically triaged with a health professional. |
| Initial investigations initiated by GP | For patients who do not need a prompt referral, all investigations should be completed, and a path of action decided, within 4 weeks of first presentation. | |
| Referral to specialist | Patients should be referred to a specialist:
|
|
| Diagnosis, staging and treatment planning | Diagnosis and staging | Timing of diagnostic investigations should be guided by the initial severity of symptoms. Staging should be completed within 4 weeks. |
| Multidisciplinary team meeting and treatment planning | A multidisciplinary team discussion is necessary and should be conducted before implementing treatment. | |
| Treatment | Watchful waiting | Watchful waiting may be recommended for asymptomatic advanced stage MZL. Watchful waiting may also be recommended for stage II FL that is not amendable to radiation therapy and advanced stage FL (stages III and IV) based on symptoms and disease bulk. Also recommended for indolent subtype of MCL. |
| Radiation therapy | Radiation should be considered in limited stage FL, in specific extranodal organ involvement (e.g. MZL of stomach, orbit) and for symptom control. Where appropriate, radiation therapy should begin within 4 weeks. | |
| Systemic therapy | In FL and MZL, the decision of when to start systemic therapy is guided by the presence of symptoms and organ dysfunction. Most MCL patients should begin treatment with systemic therapy within 2 weeks of completing staging. |
Seven steps of the optimal care pathway
Step 1: Prevention and early detection
Step 2: Presentation, initial investigations and referral step
Step 3: Diagnosis, staging and treatment planning
Step 4: Treatment
Step 5: Care after initial treatment and recovery
Step 6: Managing refractory, relapsed, residual or progressive disease
Step 7: End-of-life care
Scope of the optimal care pathway for people with low-grade lymphomas Low-grade lymphomas are a heterogenous group of generally slow-growing non-Hodgkin B-cell lymphomas (NHL), which represent about 40 per cent of all NHL.
This optimal care pathway will cover follicular lymphoma (FL), marginal zone lymphoma (MZL) and mantle cell lymphoma (MCL). With respect to other low-grade lymphoma subtypes, small
lymphocytic lymphoma is being addressed as part of the chronic lymphocytic leukaemia optimal care pathway, while Waldenström’s macroglobulinaemia and hairy cell leukaemia may be addressed in a future optimal care pathway, noting that many of the principles outlined in this document are relevant to these lymphomas.
Follicular lymphoma – World Health Organization grades 1–3A
FL is the second most common subtype of NHL. FL makes up 20–30 per cent of all NHL and can progress to become diffuse large B-cell lymphoma in approximately 10 per cent of patients during their disease course.
Marginal zone lymphoma
MZL accounts for approximately 8 per cent of all NHL.
The three main types of MZL are distinct clinical entities with specific diagnostic criteria and different genetic features, clinical behaviour and therapeutic implications (ESMO 2020):
- extranodal or mucosa-associated lymphoid tissue (MALT) lymphoma (this is the most common form of MZL, accounting for around two-thirds of all MZL)
- splenic MZL (SMZL) accounts for around 20 per cent of all MZL
- nodal MZL (NMZL) accounts for about 10 per cent of all
Mantle cell lymphoma
MCL is a rare subtype of low-grade lymphoma and may behave either as an aggressive disease or more slowly.
Low-grade lymphomas are traditionally perceived as ‘incurable’ lymphomas. However, many patients survive for more than 20 years and, given low-grade lymphomas are commonly diagnosed late in life, it may not significantly impact on their pre-morbid survival expectations.
Patients diagnosed with low-grade lymphomas will, in most cases, enter into lifelong follow-up, may have periods during which their lymphoma is monitored and not treated, and may need multiple different treatments for their lymphoma over their lifetime. While for many the truly slow-growing nature of the disease may mean patients die from other causes, in some patients the cause of death will be due to their lymphoma, and in a minority due to an aggressive change in their disease behaviour, called histologic transformation.
Noting the often-long trajectory that patients travel with their disease, this optimal care pathway focuses on pathways that enable the patient and their clinician to finesse a personalised approach that balances depth and duration of remission with treatment toxicity, optimising both duration and quality of life.
This step outlines recommendations for the prevention and early detection of low-grade lymphomas.
Evidence shows that not smoking, avoiding or limiting alcohol intake, eating a healthy diet, maintaining a healthy body weight, being physically active, being sun smart and avoiding exposure to oncoviruses or carcinogens may help reduce cancer risk (Cancer Council Australia 2018).
The causes of most low-grade lymphomas are not fully understood, and there are currently no clear prevention strategies. Some low-grade lymphomas such as gastric MALT are, however, preventable through identification and eradication of Helicobacter pylori infection.
The risk factors in common across all low-grade indolent lymphomas include the following:
- Age – incidence of low-grade lymphomas increases with age
- Obesity – high BMI in adulthood and early adulthood may increase the risk of low-grade lymphomas (Abar et al. 2019)
- Family history – individuals with a first-degree relative (parent, child, sibling) with a low-grade lymphoma have a small increased risk of developing NHL
- Race/ethnicity – there is a higher incidence of indolent NHL in white Caucasian populations compared with non-Caucasian ethnicities
- Radiation exposure – patients treated with radiation for other cancers have slightly increased risk of developing a low-grade This risk is greater for patients treated with both radiation therapy and chemotherapy
- Weakened immune system – people with weakened immune systems as a result of immunosuppressive drugs, chronic infection or some genetically inherited syndromes are at a higher risk of developing a low-grade lymphoma
- Autoimmune diseases – people with autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, Sjogren’s disease and coeliac disease may have an increased risk of developing a low-grade lymphoma
- There is a possible association between exposure to glyphosate-based agricultural pesticides and risk of developing a low-grade lymphoma, but a lack of prospective studies limits definitive
Follicular lymphoma
- Gender – women have a slightly higher risk of developing FL than men
- Race/ethnicity – FL occurs more commonly in Caucasian populations
- Viral infections – viruses that have been implicated in developing FL include Epstein-Barr virus, human T-cell lymphotropic virus type I and Kaposi sarcoma-associated herpesvirus
MALT lymphomas
MALT lymphomas, in particular, are associated with a variety of infectious/autoimmune disorders:
- 90 per cent of gastric MALT lymphoma are associated with Helicobacter pylori gastritis
- Ocular adnexal MALT lymphoma may be associated with Chlamydia psittaci
- Cutaneous MALT lymphoma may be associated with Borrelia burgdorferi
- MALT lymphoma of the small intestine and immunoproliferative small intestine disease may be associated with Campylobacter jejuni
- Thyroid MALT may be associated with Hashimoto’s thyroiditis
- Salivary gland MALT may be associated with Sjogren’s syndrome
- SMZL may be more common in those with chronic hepatitis C infection and associated with autoimmune conditions such as haemolytic anaemia and immune
Mantle cell lymphoma
- Gender – men have a greater risk of developing MCL than
Everyone should be encouraged to reduce their modifiable risk factors for cancer, including preventing and/or reducing obesity, alcohol consumption, tobacco smoking and exposure to pesticides, which may be associated with slight increased risk.
A thorough family history for NHL is recommended but no specific genetic tests are recommended.
Based on current evidence, screening is not appropriate for low-grade lymphomas.
Routine screening for lgl is not currently recommended in either the general population or in relatives of people with lgl.
This step outlines the process for the general practitioner to initiate the right investigations and refer to the appropriate specialist in a timely manner. The types of investigations the general practitioner undertakes will depend on many factors, including access to diagnostic tests, the availability of medical specialists and patient preferences.
Low-grade lymphomas frequently present with symptoms of gradual onset occurring over many weeks or several months. People can often be asymptomatic at diagnosis, with low-grade lymphomas discovered incidentally after imaging or laboratory tests reveal an abnormality.
The following signs and symptoms should be investigated:
- a lump or mass in any organ
- lymphadenopathy, particularly lymphadenopathy persistent beyond two weeks
- splenomegaly with or without systemic symptoms in the absence of, or after resolution of, any infection
- one or more of these systemic symptoms even in the absence of lymphadenopathy: fever, drenching night sweats, unexplained weight loss, frequent infections
- unexplained cytopenias
- persistent
The presence of multiple signs and symptoms, particularly in combination with other underlying risk factors, suggesting lymphoma should be considered more prominently in the differential diagnosis.
Presenting symptoms should be promptly and clinically triaged with a general practitioner.
Patients suspected to have lymphoma, based on the clinical assessment during the initial general practitioner visit, should be immediately referred to a specialist for diagnosis.
For patients where there is a lower index of suspicion, further examinations/investigations by the general practitioner should include (but are not limited to):
- a thorough history and physical examination of the skin, all lymph node groups, oral examination for enlarged Waldeyer’s ring, abdominal examination and cardiorespiratory examination
- blood tests to assess organ dysfunction including: full blood count, urea, electrolytes, creatinine, liver function tests, lactate dehydrogenase (LDH); other tests may include beta-2 microglobulin (no laboratory test can exclude these lymphomas)
- imaging of the affected area including ultrasound, chest radiography and computed tomography (CT) scan as appropriate
- biopsy as appropriate, depending on local access (referral to a specialist prior to biopsy may be appropriate where there is a high clinical suspicion for lymphoma)
- fine-needle aspiration (FNA) is generally considered inadequate for diagnosing low-grade lymphomas but in some instances may be an appropriate initial investigation (e.g. in evaluating an enlarged lymph node when a non-haemopoietic neoplasm is strongly suspected (such as head and neck cancer).
Indicators of concern that should lead to prompt referral to a specialist include:
- symptoms or results indicating organ dysfunction and low blood counts
- symptoms that suggest neurological involvement
- markedly elevated LDH
- marked B symptoms (weight loss > 10 per cent, persistent fevers > 38°C, or persistent drenching night sweats).
For patients who do not need a prompt referral to a specialist, all investigations should be completed, and a path of action decided, within four weeks of first presentation.
If a low-grade lymphoma diagnosis is confirmed by biopsy, the general practitioner must refer the patient to a haematologist or medical oncologist with professional expertise in lymphoma management. If the general practitioner considers the likelihood of lymphoma as high based on
the initial consultation, referral for urgent tissue diagnosis and ongoing management at a specialist centre with access to lymphoma multidisciplinary team support should occur.
Patients should be enabled to make informed decisions about their choice of specialist and health service. General practitioners should make referrals in consultation with the patient after considering the clinical care needed, cost implications (see referral choices and informed financial consent on page 9), waiting periods, location and facilities, including discussing the patient’s preference for health care through the public or the private system.
Referral documentation for a suspected low-grade lymphoma should incorporate appropriate documentation to allow accurate triage regarding the level of clinical urgency. Where there is clinical urgency as indicated by the features described (see 2.1.1 Timeframe for general practitioner consultation), contact the relevant specialist for advice and to ensure prompt consultation.
Documentation includes:
- important psychosocial history and relevant past history, family history, current medications and allergies
- results of current clinical investigations (imaging and pathology reports)
- results of all prior relevant investigations including imaging
- notification if an interpreter service is
Many services will reject incomplete referrals, so it is important that referrals comply with all relevant health service criteria.
If access is via online referral, a lack of a hard copy should not delay referral.
The specialist should provide timely communication to the general practitioner about the consultation and should notify the general practitioner if the patient does not attend appointments.
Aboriginal and Torres Strait Islander patients will need a culturally appropriate referral. To view the optimal care pathway for Aboriginal and Torres Strait Islander people and the corresponding quick reference guide, visit the Cancer Australia website. Download the consumer resources – Checking for cancer and Cancer from the Cancer Australia website.
For patients with indicators of concern such as organ dysfunction or neurological involvement, urgent referral to a specialist centre is needed. Specialist healthcare providers should provide clear routes of rapid access to specialist evaluation to ensure patients with indicators of concern (outlined above) are contacted and reviewed urgently.
Where lymphoma is identified by biopsy or strongly suspected, referral to specialist should occur within 72 hours.
Where there are no indicators of concern, the initial investigations outline above should take place and referral to a specialist should occur within four weeks.
The patient’s general practitioner should consider an individualised supportive care assessment where appropriate to identify the needs of an individual, their carer and family. Refer to appropriate support services as required, keeping in mind the long duration with which patients live with low- grade lymphomas. See validated screening tools mentioned in Principle 4 ‘Supportive care’.
A number of specific needs may arise for patients at this time:
- assistance for dealing with the emotional distress and/or anger of dealing with a potential cancer diagnosis, anxiety/depression, interpersonal problems and adjustment difficulties (this should include assessment of existing coping strategies and abilities to identify the needs for the patient, their carer and family)
- management of physical symptoms including pain, nausea and fatigue
- encouragement and support to increase levels of exercise (Cormie et 2018; Hayes et al. 2019)
- assessment of health literacy for self-care early in the diagnosis
- identifying impairments and providing targeted interventions to improve the patient’s function level (Silver & Baima 2013)
- an integrated and structured approach to self-care enquiry – identifying Social Health, Exercise, Education, Diet and Sleep Hygiene (SEEDS) is one such practical tool (Arden 2015)
- psycho-oncology support to improve their knowledge and motivation towards healthy self-care care behaviours and to emotionally regulate throughout the course of the disease and treatments (this is particularly the case in patients on a ‘watch and wait’ approach, which can be associated with significant stress and anxiety)
- reviewing the patient’s medication to ensure optimisation and to improve adherence to medicine used for comorbid conditions
- nutritional assessment and
See validated screening tools mentioned in Principle 4 ‘Supportive care’.
For more information refer to the National Institute for Health and Care Excellence 2015 guidelines, Suspected cancer: recognition and referral .
For additional information on supportive care and needs that may arise for different population groups, see Appendices A, B and C.
The general practitioner is responsible for:
- providing patients with information that clearly describes to whom they are being referred, the reason for referral and the expected timeframes for appointments
- requesting that patients notify them if the specialist has not been in contact within the expected timeframe
- considering referral options for patients living rurally or remotely
- supporting the patient while waiting for the specialist appointment (Cancer Council 13 11 20, Leukaemia Foundation 1800 620 420 and Lymphoma Australia 1800 953 081 are available to act as a point of information and reassurance during the anxious period of awaiting further diagnostic information).
More information
Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
Step 3 outlines the process for confirming the diagnosis and stage of cancer and for planning subsequent treatment. The guiding principle is that interaction between appropriate multidisciplinary team members should determine the treatment plan.
The treatment team, after taking a thorough medical history and making a thorough medical examination of the patient, should undertake the following investigations under the guidance of a specialist.
A definitive tissue diagnosis is always required before initiating lymphoma-specific treatment. Biopsy may have been performed before referral. Both fresh and fixed tissue samples should be collected from the tissue biopsy for anatomical pathology and potentially flow cytometry, cytogenetics and gene mutation testing (e.g. TP53 mutation testing for MCL). Additional immunohistochemical stains may in the future provide information that affects therapy (e.g. Ki67 for FL).
Lymph node architecture is a key part of the pathological examination and therefore excisional biopsy is the preferred biopsy method where possible. Where excision biopsy or large incisional biopsy is not possible, a core needle biopsy that samples the maximum number of cores with the largest calibre possible should be considered (NICE 2016).
FNA is not suitable for diagnosing lymphomas (Armitage et al. 2017). However, FNA may be an appropriate investigation in circumstances where excision or needle core biopsy is overly invasive or unfeasible (e.g. mediastinal disease). Construction of tissue blocks from cytological samples may aid diagnosis.
For low-grade lymphomas, surgery is a diagnostic procedure and rarely therapeutic. Therefore, the least invasive surgical method is recommended for diagnosis. If a highly invasive or extensive surgical procedure is being considered, consultation with the lymphoma multidisciplinary team is required.
Pathology specimens should be reviewed by a pathologist with expertise in diagnosing low-grade lymphomas. This should be done at the treatment centre conducting the MDM, before a treatment plan has been instituted.
Additional blood tests – B2M, immunoglobulins, serum protein electrophoresis – are part of the diagnostic work-up.
Evaluate relevant organ function based on history, clinical examination and, where appropriate, laboratory or imaging investigations (cardiac, respiratory, renal, hepatic). Autoimmune screens are sometimes warranted in MZL, specifically autoimmune haemolytic anaemia.
Test for occult or latent infections (e.g. HIV, hepatitis B and C, tuberculosis) that may be affected by therapy or pose a risk of reactivation due to the immunosuppressive effects of treatment. For MZL, site-specific infectious disease testing should be performed.
After receiving a referral for suspected lymphoma, the referral should be triaged accordingly, on the basis of presence of indicators of concern such as B symptoms or organ dysfunction. The timing of diagnostic investigations should be guided by the initial severity of symptoms. Staging (see 3.2 Staging and prognostic assessment) should be completed within four weeks.
Currently there are no genetic tests applicable to predict family risk of low-grade lymphomas.
Staging is a critical element in treatment planning and should be clearly documented in the patient’s medical record.
A number of lymphoma prognostic indices have been developed for the different low-grade lymphoma entities and are documented in the relevant guidelines (BSH 2020; Cheah et al., 2019; Dreyling et al. 2017; 2020). It is appropriate to document the relevant low-grade lymphoma prognostic indices at diagnosis, which may assist in the therapeutic approach.
The disease stage based on the 2014 Lugano classification (Cheson 2014) should be determined in all patients according to evidence-based guidelines.
Staging and prognostic assessment for low-grade lymphomas involves the following:
- Clinical examination and history for assessment of B It is particularly important to document the sites and extent of FL involvement that are not easily visible on imaging (e.g. skin, conjunctiva)
- Imaging with PET-CT should be performed for the staging of indolent lymphomas, in particular FL and PET-CT has greater sensitivity than CT in detecting nodal and extranodal involvement and is valuable in identifying true stage I disease amenable to radiation therapy.
Some cases of MZL exhibit low positivity on PET-CT scanning and in these instances subsequent imaging with CT may be preferable
- The decision to do a bone marrow biopsy should be according to evidence-based guidelines for the specific A bone marrow aspirate and trephine is an element of complete staging of most low-grade lymphomas. However, it may not be necessary at diagnosis where the planned initial approach is watch and wait, nor before starting treatment if the results before and/or after treatment will not impact on prognosis or therapeutic approach. The purpose of the bone marrow biopsy should be clearly explained to the patient, especially when performed in a clinical trial where it may not otherwise have been indicated
- For MCL, symptoms that suggest gastrointestinal involvement should be investigated with gastroscopy and colonoscopy
- Endoscopic ultrasound for gastric MZL can be used to characterise gastric wall infiltration and peri-gastric lymph node involvement
- MRI imaging is of value in orbital/ocular adnexa MZL
- Additional tests are recommended to calculate the relevant prognostic scores for each low-grade
Patient performance status is a central factor in cancer care and should be clearly documented in the patient’s medical record.
Performance status should be measured and recorded using an established scale such as the Karnofsky scale or the Eastern Cooperative Oncology Group (ECOG) scale.
Performance status should be recorded for both presentation and pre-morbid assessment. Consider using a validated geriatric assessment tool.
A number of factors should be considered at this stage:
- the patient’s overall condition, life expectancy, personal preferences and decision-making capacity
- discussing the multidisciplinary team approach to care with the patient
- appropriate and timely referral to an MDM
- pregnancy and fertility
- support with travel and accommodation
- teleconferencing or videoconferencing as required
- additional tests to calculate the relevant prognostic scores for each low-grade lymphoma
- evaluation of relevant organ function based on history, clinical examination and, where appropriate, laboratory or imaging investigations (cardiac, respiratory, renal, hepatic)
- autoimmune screens (these are sometimes warranted in MZL, specifically autoimmune haemolytic anaemia)
- tests for occult infections (e.g. HIV, hepatitis B and C, tuberculosis) that may be affected by therapy or pose a risk of reactivation due to the immunosuppressive effects of For MZL, site-specific infectious disease testing should be performed.
The multidisciplinary team should meet to discuss newly diagnosed patients before definitive treatment so that a treatment plan can be recommended and there can be early preparation for the post-treatment phase. The level of discussion may vary, depending on the patient’s clinical and supportive care factors. The proposed treatment must be recorded in the patient’s medical record and should be recorded in an MDM database where one exists.
Results of all relevant tests and access to images should be available for the MDM. Information about the patient’s concerns, preferences and social and cultural circumstances should also be available.
Specifically in low-grade lymphomas, ‘watch and wait’, the dynamic observation of asymptomatic disease, can lead to significant anxiety. The patient’s anxiety can be alleviated with education from the treating specialist and counselling from a psychologist with experience in lymphoma.
See validated screening tools mentioned in Principle 4 ‘Supportive care’.
A number of specific challenges and needs may arise for patients at this time:
- assistance for dealing with psychological and emotional distress while adjusting to the diagnosis; treatment phobias; existential concerns; stress; difficulties making treatment decisions; anxiety or depression or both; psychosexual issues such as potential loss of fertility and premature menopause; history of sexual abuse; and interpersonal problems
- management of physical symptoms such as pain and fatigue (Australian Adult Cancer Pain Management Guideline Working Party 2019)
- malnutrition or undernutrition, identified using a validated nutrition screening tool such as the MST (note that many patients with a high BMI [obese patients] may also be malnourished [WHO 2018])
- support for families or carers who are distressed with the patient’s cancer diagnosis
- support for families/relatives who may be distressed after learning of a genetically linked cancer diagnosis
- specific spiritual needs that may benefit from the involvement of pastoral/spiritual care. Additionally, palliative care may be required at this
For more information on supportive care and needs that may arise for different population groups, see Appendices A, B and C.
The multidisciplinary team should be composed of the core disciplines that are integral to providing good care. Team membership should reflect both clinical and supportive care aspects of care.
Pathology and radiology expertise are essential.
See Appendix E for a list of team members who may be included in the multidisciplinary team for low-grade lymphomas.
Core members of the multidisciplinary team are expected to attend most MDMs either in person or remotely via virtual mechanisms. Additional expertise or specialist services may be required for some patients. An Aboriginal and Torres Strait Islander cultural expert should be considered for all patients who identify as Aboriginal or Torres Strait Islander.
The general practitioner who made the referral is responsible for the patient until care is passed to another practitioner who is directly involved in planning the patient’s care.
The general practitioner may play a number of roles in all stages of the cancer pathway including diagnosis, referral, treatment, shared follow-up care, post-treatment surveillance, coordination and continuity of care, as well as managing existing health issues and providing information and support to the patient, their family and carer.
A nominated contact person from the multidisciplinary team may be assigned responsibility for coordinating care in this phase. Care coordinators are responsible for ensuring there is continuity throughout the care process and coordination of all necessary care for a particular phase (COSA 2015). The care coordinator may change over the course of the pathway.
The lead clinician is responsible for overseeing the activity of the team and for implementing treatment within the multidisciplinary setting.
Patients should be encouraged to participate in research or clinical trials where available and appropriate.
Participation in clinical trials, patient registries and tissue banking, where available, is encouraged for patients with low-grade lymphomas. Cross-referral between clinical trials centres should be encouraged to facilitate participation.
For more information visit:
Cancer prehabilitation uses a multidisciplinary approach combining exercise, nutrition and psychological strategies to prepare patients for the challenges of cancer treatment such as systemic therapy and radiation therapy. Team members may include anaesthetists, oncologists, surgeons, haematologists, nurses, clinical psychologists, exercise physiologists, physiotherapists and dietitians, among others.
For patients with low-grade lymphomas who may undergo multiple treatments over many decades, prehabilitation may be an ongoing intervention that becomes increasingly relevant as the patient ages and experiences additional medical, physical and psychological limitations.
Patient performance status is a central factor in cancer care and should be frequently assessed. All patients should be screened for malnutrition using a validated tool such as the Malnutrition Screening Tool (MST). The lead clinician should refer obese or malnourished patients to a dietitian preoperatively or before other treatments begin.
Patients who currently smoke should be encouraged to stop smoking before receiving or during treatment. This can include an offer of referral to Quitline in addition to smoking cessation pharmacotherapy if clinically appropriate.
Evidence in solid cancers indicates that patients who respond well to prehabilitation may have fewer complications after treatment. For example, those who were exercising before diagnosis and patients who use prehabilitation before starting treatment may improve their physical or psychological outcomes, or both, and this helps patients to function at a higher level throughout their cancer treatment (Cormie et al. 2017; Silver 2015).
For patients with low-grade lymphomas, including those who will initially undergo close observation in a ‘watch and wait’ approach, the multidisciplinary team should consider these specific prehabilitation assessments and interventions:
- conducting a physical and psychological assessment to establish a baseline function level, including assessing coping strategies/abilities
- identifying impairments and providing targeted interventions to improve the patient’s function level (Silver & Baima 2013)
- an integrated and structured approach to self-care enquiry – identifying Social Health, Exercise, Education, Diet and Sleep Hygiene (SEEDS) is one such practical tool (Arden 2015)
- referral to a psycho-oncology service to improve their knowledge and motivation towards healthy self-care care behaviours and to emotionally regulate throughout the course of the disease and treatments
- reviewing the patient’s medication to ensure optimisation and to improve adherence to medicine used for comorbid conditions.
Following completion of primary cancer treatment, rehabilitation programs have considerable potential to enhance physical function.
Cancer and cancer treatment may cause fertility problems. This will depend on the age of the patient, the type of cancer and the treatment received. Infertility can range from difficulty having a child to the inability to have a child. Infertility after treatment may be temporary, lasting months to years, or permanent (AYA Cancer Fertility Preservation Guidance Working Group 2014).
Patients need to be advised about and potentially referred for discussion about fertility preservation before starting treatment and need advice about contraception before, during and after treatment. Patients and their family should be aware of the ongoing costs involved in optimising fertility. Fertility management may apply in both men and women. Fertility preservation options are different for men and women and the need for ongoing contraception applies to both men and women.
The potential for impaired fertility should be discussed and reinforced at different time points as appropriate throughout the diagnosis, treatment, surveillance and survivorship phases of care. These ongoing discussions will enable the patient and, if applicable, the family to make informed decisions. All discussions should be documented in the patient’s medical record.
More information
See the Cancer Council website for more information.
See validated screening tools mentioned in Principle 4 ‘Supportive care’.
A number of specific challenges and needs may arise for patients at this time:
- assistance for dealing with psychological and emotional distress while adjusting to the diagnosis; stigma; treatment phobias; existential concerns; stress; difficulties making treatment decisions; anxiety or depression or both; psychosexual issues such as potential loss of fertility and premature menopause; history of sexual abuse; and interpersonal problems
- physical distress caused by breathlessness and coughing, which may be alleviated through a referral to allied health professionals (physiotherapy, occupational therapy, exercise physiology or pulmonary rehabilitation); non-pharmacological strategies may be beneficial in breathlessness management (CareSearch 2019a) (note: if oxygen is medically indicated, this can be arranged through the relevant state aids and equipment program)
- hoarseness may require referral to a speech therapist or ENT specialist for palliative procedures
- management of physical symptoms such as pain, fatigue, cough and breathlessness (Australian Adult Cancer Pain Management Guideline Working Party 2019; Johnson & Currow 2016)
- delays in help-seeking for symptoms and psychological distress due to stigmatisation of Low-Grade Lymphomas associated with smoking (Cancer Australia 2020b)
- having issues with family and friends because of the association of tobacco use and Low-Grade Lymphomas (Carmack Taylor et al. 2008)
- malnutrition or undernutrition, identified using a validated nutrition screening tool such as the MST (note that many patients with a high BMI [obese patients] may also be malnourished [WHO 2018])
- support for families or carers who are distressed with the patient’s cancer diagnosis
- support for families/relatives who may be distressed after learning of a genetically linked cancer diagnosis
- specific spiritual needs that may benefit from the involvement of pastoral/spiritual care.
Additionally, palliative care may be required, particularly following an advanced stage Low-Grade Lymphomas diagnosis (stages III–IV) or to assist with pain management.
For more information on supportive care and needs that may arise for different population groups, see Appendices A and B, and special population groups.
In discussion with the patient, the lead clinician should undertake the following:
- establish if the patient has a regular or preferred general practitioner and if the patient does not have one, then encourage them to find one
- provide written information appropriate to the health literacy of the patient about the diagnosis and treatment to the patient and carer and refer the patient to the Guide to best cancer care (consumer optimal care pathway) for low-grade lymphomas as well as to relevant websites and support groups such as Cancer Council, the Leukaemia Foundation.
- provide a treatment care plan including contact details for the treating team and information on when to call the hospital
- discuss a timeframe for diagnosis and treatment with the patient and carer
- explain the principles of ‘watch and wait’ if active surveillance is planned rather than commencing treatment
- discuss the benefits of multidisciplinary care and gain the patient’s consent before presenting their case at an MDM
- discuss progress in the cycle of quitting and refer to Quitline (13 7848) for behavioural intervention if the patient currently smokes (or has recently quit), and prescribe smoking cessation pharmacotherapy, as clinically appropriate
- recommend an ‘integrated approach’ throughout treatment regarding nutrition, exercise, sleep hygiene, cognitive function (commonly affected by steroids) and minimal or no alcohol consumption, among other considerations
- communicate the benefits of continued engagement with primary care during treatment for managing comorbid disease, health promotion, care coordination and holistic care
- where appropriate, review fertility needs with the patient and refer for specialist fertility management (including fertility preservation, contraception, management during pregnancy and of future pregnancies)
- be open to and encourage discussion about the diagnosis, prognosis (if the patient wishes to know) and survivorship and palliative care while clarifying the patient’s preferences and needs, personal and cultural beliefs and expectations, and their ability to comprehend the communication
- encourage the patient to participate in advance care planning including considering appointing one or more substitute decision-makers and completing an advance care directive to clearly document their treatment Each state and territory has different terminology and legislation surrounding advance care directives and substitute decision-makers.
The lead clinician has these communication responsibilities:
- involving the general practitioner from the point of diagnosis
- ensuring regular and timely communication with the general practitioner about the diagnosis, treatment plan and recommendations from MDMs and inviting them to participate in MDMs (consider using virtual mechanisms)
- supporting the role of general practice both during and after treatment
- discussing shared or team care arrangements with general practitioners or regional cancer specialists, or both, together with the patient.
More information
Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
Step 4 describes the optimal treatments for low-grade lymphomas, the training and experience required of the treating clinicians and the health service characteristics required for optimal cancer care.
All health services must have clinical governance systems that meet the following integral requirements:
- identifying safety and quality measures
- monitoring and reporting on performance and outcomes
- identifying areas for improvement in safety and quality (ACSQHC 2020).
Step 4 outlines the treatment options for low-grade lymphomas. For detailed clinical information on treatment options refer to these resources:
- ESMO 2020: Follicular lymphoma: a guide for patients
- BSH 2020: Guideline on the investigation and management of follicular lymphoma
- Trotman et 2019: Front-line management of indolent NHL in Australia. Part 1: Follicular lymphoma
- Cheah et al. 2019: Front line management of indolent non Hodgkin lymphoma in Australia. Part 2: mantle cell lymphoma and marginal zone lymphoma.
The intent of treatment can be defined as one or more of the following, which are not exclusive:
- curative
- improvement in quality of life and/or longevity with close observation, initiation of local or systemic therapy or a combination
- symptom
The treatment intent should be established in a multidisciplinary setting, documented in the patient’s medical record and conveyed to the patient and carer as appropriate.
The potential benefits need to be balanced against the morbidity and mortality risks of treatment.
The lead clinician should discuss the proposed treatment program, including advantages and disadvantages of each treatment and associated potential side effects with the patient and their carer or family before treatment consent is obtained and begins so the patient can make an informed decision. Supportive care services should also be considered during this decision-making process.
Patients should be asked about their use of (current or intended) complementary therapies (see Appendix D).
Timeframes for starting treatment should be informed by evidence-based guidelines where they exist. The treatment team should recognise that shorter timeframes for appropriate consultations and starting therapy can promote a better experience for patients.
Initiate advance care planning discussions with patients before treatment begins (this could include appointing a substitute decision-maker and completing an advance care directive). Formally involving a palliative care team/service may benefit any patient, so it is important to know and respect each person’s preference (Australian Government Department of Health 2021a).
The current recommended therapeutic approach is based on the type of low-grade lymphoma, clinical risk factors, presence of symptoms and patient perspective (ESMO 2020).
See the following Australian, British and European guidelines for detailed information regarding therapies.
- Front-line management of indolent non-Hodgkin lymphoma in Australia
- Non-Hodgkin’s lymphoma: Diagnosis and management: NICE guidelines
- Newly diagnosed and relapsed follicular lymphoma: ESMO clinical practice guidelines
- Newly diagnosed and relapsed mantle cell lymphoma: ESMO clinical practice guidelines
For stage II FL (non-contiguous lymph nodes, or not amenable to radiation therapy) and advanced stage FL (stages III and IV), the decision to start treatment is guided by symptoms and disease bulk. Approximately one-third of initial presentations occur in patients with low-volume disseminated disease. The importance of ‘watch and wait’ is true even in the modern immunochemotherapy era. The frequency of clinical review during this observation is based on the tempo of the disease, the comfort the patient has with a ‘watch and wait’ approach and the likelihood that they will recognise and re-present in the event of signs of relapse.
Watchful waiting can cause significant anxiety in patients. Appropriate support should be made available (see 3.6.3 Supportive care). Alternate approaches such as treatment with rituximab monotherapy may delay the need for subsequent treatment.
Asymptomatic advance-stage nodal MZL can also be managed with a watchful waiting approach.
An indolent form of MCL, commonly a leukaemic presentation, indicated by lack of symptoms and low tumour burden, can be followed with watchful waiting.
Radiation therapy has an important role in specific scenarios within indolent lymphoma subtypes:
- Early-stage FL (stage I and stage II in which lymph nodes are contiguous) is potentially curable with radiation Further adjuvant immunochemotherapy may confer additional progression-free survival
- In centres with radiation expertise, there may be a role for curative radiation therapy (total nodal irradiation) in a highly select group of patients with low-volume, advanced-stage disease
- Radiation therapy is appropriate in early-stage MZL (including gastric, cutaneous, unilateral and bilateral orbital MALT, and other localised MZLs) with potential curative intent. Note eradication of Helicobacter pylori infection should be performed first – it may induce remission without the need for radiation therapy in some cases
- In localised relapse of low-grade lymphomas, it may defer the need for systemic immunochemotherapy
- It may be used for symptom control in advanced-stage low-grade lymphomas, where lymphoma is impairing quality of life.
Timeframe for starting treatment
Begin within four weeks, as prioritised by a multidisciplinary team decision (see 3.4 Treatment planning). Start earlier for life- or organ-threatening indications. Delaying radiation therapy (e.g. for further monitoring) may cause distress and should be discussed with the patient.
Training and experience required of the appropriate specialists
Fellow of the Royal Australian and New Zealand College of Radiologists or equivalent, with adequate training and experience, institutional credentialing and agreed scope of practice in lymphoma management.
The training and experience of the radiation oncologist should be documented.
Health service unit characteristics
To provide safe and quality care for patients having radiation therapy, health services should have these features:
- linear accelerator (LINAC) capable of image-guided radiation therapy (IGRT)
- dedicated CT planning
- access to MRI and PET imaging
- automatic record-verify of all radiation treatments delivered
- a treatment planning system
- trained medical physicists, radiation therapists and nurses with radiation therapy experience
- coordination for combined therapy with systemic therapy, especially where facilities are not co-located
- participation in Australian Clinical Dosimetry Service audits
- an incident management system linked with a quality management
Systemic therapy is appropriate in most patients with non-contiguous stage II or stage III–IV disease who are symptomatic by GELF/BCNI criteria, and considered fit enough to experience a positive risk-benefit balance of undergoing treatment (Ardeshna et al. 2003; Brice et al. 1997). The choice of initial systemic therapy needs to consider the potential for sequencing of subsequent therapies, including potential future stem cell mobilisation.
Follicular lymphoma
Initial treatment with chemotherapy and anti-CD20 monoclonal antibody is often followed by continued therapy with anti-CD20 antibody maintenance for another two years. Given that ongoing maintenance antibody therapy increases progression-free survival but does not prolong overall survival, it is important the patient understands both the benefits in prolonging remission as well as the additional infectious toxicities of using maintenance antibody therapy.
Nodal marginal zone lymphoma
Initial treatment with chemotherapy and anti-CD20 monoclonal antibody is recommended.
Extranodal marginal zone lymphoma
Helicobacter pylori eradication therapy should be given to all patients with gastric MALT, irrespective of stage and Helicobacter pylori status. In those who remain Helicobacter pylori positive, second- line eradication therapy is recommended. Regression of lymphoma following successful eradication of Helicobacter pylori may be delayed, and so it is appropriate to wait 12 months before starting another treatment.
In other instances of localised MALT (e.g. conjunctival MALT), a trial of systemic therapy with antibiotics may be appropriate before radiation therapy.
MALT can also be treated with chemotherapy and anti-CD20 monoclonal antibody.
Splenic marginal zone lymphoma
Recognised first-line therapeutic options are rituximab monotherapy, splenectomy (after appropriate vaccinations) or chemotherapy and anti-CD20 monoclonal antibody combinations. While half of splenectomised patients do not need further treatment for SMZL, splenectomy may bring about complications and is increasingly being replaced with rituximab +/- chemotherapy as initial therapy, especially in patients with a heavy bone marrow disease burden.
Mantle cell lymphoma
MCL causing symptoms should be treated with systemic chemotherapy and anti-CD20 monoclonal antibody combination, incorporating high-dose cytarabine in younger, fitter patients, followed by consolidation with autologous stem cell transplantation (ASCT). Rituximab maintenance after ASCT has been shown to improve overall survival.
In older, more frail patients, chemotherapy and anti-CD20 monoclonal antibody combinations is appropriate. Where bendamustine-containing regimens are used, meticulous monitoring for infections is necessary.
Timeframes for starting treatment
The decision to start treatment may occur after a long period of watch and wait. In FL and MZL, the decision of when to start systemic therapy is guided by the presence of symptoms and organ dysfunction according to the GELF/BCNI criteria. Once the patient meets the criteria to start, treatment should begin within four weeks. Most symptomatic MCL patients should begin treatment with systemic therapy within two weeks of completing staging.
Training and experience required of the appropriate specialists
The following training and experience is required of the appropriate specialist(s): Haematologists and medical oncologists must have training and experience of this standard:
- Fellow of the Royal Australian College of Physicians (or equivalent)
- adequate training and experience that enables institutional credentialing and agreed scope of practice within this area (ACSQHC 2015).
Cancer nurses should have accredited training in these areas:
- anti-cancer treatment administration
- specialised nursing care for patients undergoing cancer treatments, including side effects and symptom management
- the handling and disposal of cytotoxic waste (ACSQHC 2020).
Systemic therapy should be prepared by a pharmacist whose background includes this experience:
- adequate training in systemic therapy medication, including dosing calculations according to protocols, formulations and/or
If no haematologists or medical oncologist is locally available (e.g. regional or remote areas), some components of less complex therapies may be delivered by a general practitioner or nurse with training and experience that enables credentialing and agreed scope of practice within this area. This should be in line with a detailed treatment plan or agreed protocol, and with communication as agreed with the haematologists or medical oncologist or as clinically required.
Health service characteristics
To provide safe and quality care for patients having systemic therapy, health services should have these features:
- a clearly defined path to emergency care and advice after hours
- access to basic haematology and biochemistry testing
- cytotoxic drugs prepared in a pharmacy with appropriate facilities
- occupational health and safety guidelines for handling cytotoxic drugs, including safe prescribing, preparation, dispensing, supplying, administering, storing, manufacturing, compounding and monitoring the effects of medicines (ACSQHC 2011)
- guidelines and protocols for delivering treatment safely (including dealing with extravasation of drugs)
- coordination for combined therapy with radiation therapy, especially where facilities are not co-located
- timely access to pathology and blood
Antimicrobial prophylaxis and immunoglobulin supplementation (in hypogammaglobulinaemic patients who meet national prescribing criteria) is recommended. Specific antimicrobial prophylaxis should be prescribed based on established guidelines (national guidelines and eviQ) and the results of tests for occult or latent infection (see 3.1 Specialist diagnostic work-up). This includes, but
is not limited to, the particular risk of reactivation of latent hepatitis B associated with anti-CD20 monoclonal antibodies. Patients with hepatitis B core antibody require a documented plan for antiviral therapy and ongoing monitoring.
Yearly seasonal flu vaccination and five-yearly pneumococcal vaccination should be encouraged in accordance with the Australian National Immunisation Schedule, as should COVID vaccination boosters as/if the evolving evidence supports this approach.
The primary role of surgery in low-grade lymphomas is to obtain a biopsy specimen. Surgery is
a beneficial component of indolent lymphoma treatment in a minority of cases such as in relieving mechanical obstruction caused by lymphoma (e.g. an acute bowel obstruction in duodenal follicular lymphoma).
Splenectomy is an important therapeutic option for SMZL (see 4.2.3 Systemic therapy).
Documented evidence of the surgeon’s training and experience, including their relevant organ- specific sub-specialty experience with low-grade lymphomas and procedures to be undertaken, should be available.
Health service characteristics
To provide safe and quality care for patients having surgery, health services should have these features:
- critical care support
- 24-hour medical staff availability
- 24-hour operating room access and intensive care unit
- diagnostic imaging
- pathology
- PET
While chemoimmunotherapy has been the cornerstone of frontline treatment for advanced disease in cases of relapse, several other therapeutic strategies are under development.
Promising therapeutic agents include:
- small molecules targeting signal transduction (PI3K inhibitors, BTK inhibitors)
- monoclonal antibodies targeting other cell surface proteins (CD19, CD47)
- epigenetic modifiers (EZH2 and HDAC inhibitors)
- immune checkpoint inhibitors (PD1, PD-L1, TIGIT)
- engineered CARs (CAR T- and CAR NK-cells)
- bispecific T-cell engagers
- antibody drug conjugates
- radioimmunoconjugates
- cancer vaccines
- immunomodulatory
Many of these agents are in advanced stages of development and have proven efficacy and manageable toxicity. Clinical trial participation is a good therapeutic consideration, particularly for patients who have progressed after two lines of therapy. ASCT and sometimes allogeneic stem cell transplantation is still a good option for certain patients with relapsed disease.
Palliative care is a multidisciplinary approach to symptom management, psychosocial support and assistance in identifying care goals for patients with serious illness and their families.
Early referral to palliative care can improve the quality of life for people with cancer, improve caregiver outcomes and, in some cases, may have survival benefits (Haines 2011; Temel et al. 2010; Zimmermann et al. 2014).
The lead clinician should ensure patients receive timely and appropriate referral to palliative care services. Referral should be based on need rather than prognosis. Emphasise the value of palliative care in improving symptom management and quality of life to patients and their carers at any stage of disease. This is specifically important to explain to patients with a low-grade lymphoma and their families, due to the often lengthy course of the disease.
The ‘Dying to Talk’ resource may help health professionals when initiating discussions with patients about future care needs (see ‘More information’). Ensure that carers and families receive information, support and guidance about their role in palliative care (Palliative Care Australia 2018).
Patients, with support from their family or carer and treating team, should be encouraged to consider appointing a substitute decision-maker and to complete an advance care directive. Refer to step 6 for a more detailed description of managing patients with refractory, relapsed, residual or progressive disease.
More information
These online resources are useful:
The team should support the patient to participate in research or clinical trials where available and appropriate. Many emerging treatments are only available on clinical trials that may require referral to certain trial centres.
For more information visit:
See validated screening tools mentioned in Principle 4 ‘Supportive care’.
Patients with low-grade lymphomas may undergo another period of watchful waiting before their initial therapy and this can lead to anxieties related to the stress and uncertainty of observation. Ongoing patient education from their lymphoma specialist and, if further support is needed, a referral to a psychologist with experience in lymphoma is recommended (see 3.6.3 Supportive care).
A number of specific challenges and needs may arise for patients at this time:
- assistance for dealing with emotional and psychological issues, including body image concerns, fatigue, quitting smoking, traumatic experiences, existential anxiety, treatment phobias, anxiety/ depression, interpersonal problems and sexuality concerns
- potential isolation from normal support networks, particularly for rural patients who are staying away from home for treatment
- cognitive changes as a result of treatment (e.g. altered memory, attention and concentration)
- diet needs – these are likely to change over time during the different phases of treatment
- nutritional assessment and support for malnutrition due to ongoing treatment side effects (including weight loss, reduced oral intake and cachexia), which may require monitoring and nutrition intervention from a dietitian
- management of gastrointestinal symptoms (including vomiting, mucositis, reflux and early satiety), difficulty swallowing and decrease in appetite require optimal symptom control
- management of physical symptoms such as nausea and loss of appetite
- decline in mobility or functional status as a result of treatment
- assistance with beginning or resuming regular exercise with referral to an exercise physiologist or physiotherapist (COSA 2018; Hayes et al. 2019).
Early involvement of general practitioners may lead to improved cancer survivorship care following acute treatment. General practitioners can address many supportive care needs through good communication and clear guidance from the specialist team (Emery 2014).
Patients, carers and families may have these additional issues and needs:
- financial issues related to loss of income (through reduced capacity to work or loss of work) and additional expenses as a result of illness or treatment
- advance care planning, which may involve appointing a substitute decision-maker and completing an advance care directive
- legal issues (completing a will, care of dependent children) or making an insurance, superannuation or social security claim on the basis of terminal illness or permanent disability.
Cancer Council 13 11 20, Leukaemia Foundation 1800 620 420 and Lymphoma Australia 1800 953 081 information and support lines can assist with information and referral to local support services.
For more information on supportive care and needs that may arise for different population groups, see Appendices A, B and C.
Rehabilitation may be required at any point of the care pathway. If it is required before treatment, it is referred to as prehabilitation (see section 3.6.1).
All members of the multidisciplinary team have an important role in promoting rehabilitation. Team members may include occupational therapists, speech pathologists, dietitians, social workers, psychologists, physiotherapists, exercise physiologists and rehabilitation specialists.
To maximise the safety and therapeutic effect of exercise for people with cancer, all team members should recommend that people with cancer work towards achieving, and then maintaining, recommended levels of exercise and physical activity as per relevant guidelines. Exercise should be prescribed and delivered under the direction of an accredited exercise physiologist or physiotherapist with experience in cancer care (Vardy et al. 2019). The focus of intervention from these health professionals is tailoring evidence-based exercise recommendations to the individual patient’s needs and abilities, with a focus on the patient transitioning to ongoing self-managed exercise.
Other issues that may need to be dealt with include managing cancer-related fatigue, improving physical endurance, achieving independence in daily tasks, optimising nutritional intake, returning to work and ongoing adjustment to cancer and its consequences. Referrals to dietitians, psychosocial support, return-to-work programs and community support organisations can help in managing these issues.
The lead or nominated clinician should take responsibility for these tasks:
- discussing treatment options with patients and carers, including the treatment intent and expected outcomes, and providing a written version of the plan and any referrals
- providing patient and carers with information about the possible side effects of treatment, managing symptoms between active treatments, how to access care, self-management strategies and emergency contacts
- encouraging patients to use question prompt lists and audio recordings, and to have a support person present to aid informed decision making
- initiating a discussion about advance care planning and involving carers or family if the patient
The general practitioner plays an important role in coordinating care for patients, including helping to manage side effects and other comorbidities, and offering support when patients have questions or worries. For most patients, simultaneous care provided by their general practitioner is very important.
The lead clinician, in discussion with the patient’s general practitioner, should consider these points:
- the general practitioner’s role in symptom management, supportive care and referral to local services
- using a chronic disease management plan and mental health care management plan
- how to ensure regular and timely two-way communication about:
- the treatment plan, including intent and potential side effects
- supportive and palliative care requirements
- the patient’s prognosis and their understanding of this
- enrolment in research or clinical trials
- changes in treatment or medications
- the presence of an advance care directive or appointment of a substitute decision-maker
- recommendations from the multidisciplinary
More information
Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
The term ‘cancer survivor’ describes a person living with cancer, from the point of diagnosis until the end of life. Survivorship care in Australia has traditionally been provided to patients who have completed active treatment and are in the follow-up phase. But there is now a shift to provide survivorship care and services from the point of diagnosis to improve cancer- related outcomes.
Cancer survivors may experience inferior quality of life and cancer-related symptoms for up to five years after their diagnosis (Jefford et al. 2017). Distress, fear of cancer recurrence, fatigue, obesity and sedentary lifestyle are common symptoms reported by cancer survivors (Vardy et al. 2019).
Due to an ageing population and improvements in treatments and supportive care, the number of people surviving cancer is increasing. International research shows there is an important need
to focus on helping cancer survivors cope with life beyond their acute treatment. Cancer survivors often face issues that are different from those experienced during active treatment for cancer and may include a range issues, as well as unmet needs that affect their quality of life (Lisy et al. 2019; Tan et al. 2019).
Physical, emotional and psychological issues include fear of cancer recurrence, cancer-related fatigue, pain, distress, anxiety, depression, cognitive changes and sleep issues (Lisy et al. 2019). Late effects may occur months or years later and depend on the type of cancer treatment. Survivors and their carers may experience impacted relationships and practical issues including difficulties with return to work or study and financial hardship. They may also experience changes to sex and intimacy. Fertility, contraception and pregnancy care after treatment may require specialist input.
The Institute of Medicine, in its report From cancer patient to cancer survivor: Lost in transition, describes the essential components of survivorship care listed in the paragraph above, including interventions and surveillance mechanisms to manage the issues a cancer survivor may face
(Hewitt et al. 2006). Access to a range of health professions may be required including physiotherapy, occupational therapy, social work, dietetics, clinical psychology, fertility and palliative care.
Coordinating care between all providers is essential to ensure the patient’s needs are met.
Cancer survivors are more likely than the general population to have and/or develop comorbidities (Vijayvergia & Denlinger 2015). Health professionals should support survivors to self-manage their own health needs and to make informed decisions about lifestyle behaviours that promote wellness and improve their quality of life (Australian Cancer Survivorship Centre 2010; Cancer Australia 2017; NCSI 2015).
The transition from active treatment to post-treatment care is critical to long-term health. In some cases, people will need ongoing, hospital-based care, and in other cases a shared follow-up care arrangement with their general practitioner may be appropriate. This will vary depending on the type and stage of cancer and needs to be planned. Shared follow-up care involves the joint participation of specialists and general practitioners in the planned delivery of follow-up and survivorship care. A shared care plan is developed that outlines the responsibilities of members of the care team, the follow-up schedule, triggers for review, plans for rapid access into each setting and agreement regarding format, frequency and triggers for communication. After completing initial treatment, a designated member of the multidisciplinary team (most commonly nursing or medical staff involved in the patient’s care) should provide the patient with a needs assessment and treatment summary and develop a survivorship care plan in conjunction with the patient. This should include a comprehensive list of issues identified by all members of the multidisciplinary team involved in the patient’s care and by the patient. These documents are key resources for the patient and their healthcare providers and can be used to improve communication and care coordination. The treatment summary should cover, but is not limited to: Responsibility for follow-up care should be agreed between the lead clinician, the general practitioner, relevant members of the multidisciplinary team and the patient. This is based on guideline recommendations for follow-up care, as well as the patient’s current and anticipated physical and emotional needs and preferences. Evidence comparing shared follow-up care and specialised care indicates equivalence in outcomes including recurrence rate, cancer survival and quality of life (Cancer Research in Primary Care 2016). Ongoing communication between healthcare providers involved in care and a clear understanding of roles and responsibilities is key to effective survivorship care. In particular circumstances, other models of follow-up care can be safely added such as nurse-led models (Monterosso et al. 2019). Other models of follow-up care can be provided in these locations or by these health professionals: A designated member of the team should document the agreed survivorship care plan. The survivorship care plan or chronic disease management plan should support wellness and have a strong emphasis on healthy lifestyle changes such as a balanced diet, a non-sedentary lifestyle, weight management and a mix of aerobic and resistance exercise (COSA 2018; Hayes et al. 2019). This survivorship care plan should also cover, but is not limited to: Processes for rapid re-entry to hospital care should be documented and communicated to the patient and relevant stakeholders. Care in the initial follow-up phase is driven by predicted risks (e.g. the risk of relapse or progression, developing late effects of treatment and psychological issues) as well as individual clinical and supportive care needs. It is important that follow-up care is based on evidence and is consistent with guidelines. Not all people will require ongoing tests or clinical review and may be discharged to general practice follow-up. The lead clinician should discuss (and general practitioner reinforce) options for follow-up. It is critical for optimal aftercare that the designated member of the treatment team educates the patient about the symptoms of recurrence. General practitioners (including nurses) can: More information Templates and other resources to help with developing treatment summaries and survivorship care plans are available from these organisations: People frequently ask if there is anything they can do to reduce the risk of low grade lymphoma recurrence. Not smoking, eating a healthy diet, being sun smart, limiting (or avoiding) alcohol intake, being physically active and maintaining a healthy body weight may help reduce the risk of a second primary cancer. However, none of these factors have been shown to affect the risk of relapse for low-grade lymphomas. Encourage and support all cancer survivors to reduce modifiable risk factors for other cancers and chronic diseases. Ongoing coordination of care between providers should also deal with any comorbidities, particularly ongoing complex and life-threatening comorbid conditions. Support cancer survivors to participate in research or clinical trials where they are available and appropriate. These might include studies to understand survivors’ issues, to better manage treatment side effects, or to improve models of care and quality of life. For more information visit: Patients with low-grade lymphomas may experience multiple lines of treatment over many years and therefore benefit from reassessment of their supportive care needs: This may be encapsulated in the prehabilitation framework (see 3.6.1 Prehabilitation) and in the supportive care principles during active treatment phase (outlined in 4.5.1 Supportive care). See validated screening tools mentioned in Principle 4 ‘Supportive care’. Additionally, the ‘Cancer Survivors Unmet Needs (CaSun)’ is another validated screening tool that may help health professionals to identify the unmet needs of patients during survivorship. A number of specific challenges and needs may arise for cancer survivors: For more information on supportive care and needs that may arise for different population groups, see Appendices A, B and D. Rehabilitation may be required at any point of the care pathway from the pre-treatment phase through to disease-free survival and palliative care (Cormie et al. 2017). Issues that may need to be dealt with include managing cancer-related fatigue, coping with cognitive changes, improving physical endurance, achieving independence in daily tasks, returning to study or work and ongoing adjustment to cancer and its consequences. Exercise is a safe and effective intervention that improves the physical and emotional health and wellbeing of cancer patients. Exercise should be embedded as part of standard practice in cancer care and be viewed as an adjunct therapy that helps counteract the adverse effects of cancer and its treatment. Cancer survivors may find referral to specific cancer rehabilitation, optimisation programs or community-based rehabilitation appropriate and beneficial. Other options include referral to allied health supports through team care arrangements and mental health plans. Some community support organisations (cancer-related non-government, not-for-profit and charities) provide services to cancer survivors. The lead clinician (themselves or by delegation) should take responsibility for these tasks: The lead clinician should ensure regular, timely, two-way communication with the general practitioner about: More information Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
Patients who present with persisting residual or relapsed disease should be managed by a multidisciplinary team and offered timely referral to appropriate physical, practical and emotional support. Where that recurrence is treated in a different setting to original the previous treatment details and any toxicities needs to be obtained from the original treating centre.
Step 6 is concerned with managing residual or relapsed disease. The likelihood of such depends on many factors usually related to the type and stage of low-grade lymphomas, and the effectiveness of treatment. Many low-grade lymphomas cannot be eradicated even with the best initial treatment.
But prolonged survival through controlling disease and disease-related symptoms is normal for low-grade lymphomas. Watch and wait active surveillance of relapse, rather than immediate treatment, is commonly recommended.
Recurrent disease may be discovered by the patient or by surveillance in the post-treatment period. Symptoms can often present as:
Managing residual or relapsed disease is complex and should therefore involve all the appropriate specialties in a multidisciplinary team including palliative care where appropriate. From the time of diagnosis, the team should offer patients appropriate psychosocial care, supportive care, advance care planning and symptom-related interventions as part of their routine care. The approach should be personalised to meet the patient’s individual needs, values and preferences. The full complement of supportive care measures as described throughout the optimal care pathway and in Appendices A, B and C should be offered to assist patients and their families and carers to cope. These measures should be updated as the patient’s circumstances change. Survivorship care should be considered and offered at an early stage. Many people live with advanced cancer for many months or years. As survival is improving in many patients, survivorship issues should be considered as part of routine care. Health professionals should therefore be ready to change and adapt treatment strategies according to disease status, prior treatment tolerance and toxicities and the patient’s quality of life, in addition to the patient’s priorities and life plans. In a suspected relapse, consider conducting a biopsy to confirm the relapse. Also consider whether there are clinical features to suggest transformation to high-grade lymphoma or involvement by a different lymphoma or neoplasm. In the event of a re-biopsy, the appropriate tissue diagnostic and prognostic investigations can be undertaken again as necessary. Molecular tests may in the near future be able to guide use of novel therapies (e.g. EZH2 mutation in FL). Re-staging of relapsed or refractory disease should be performed with CT-PET scan, or if indolent disease was previously PET-negative, with CT scan. Consider a repeat bone marrow biopsy to evaluate the cause of cytopenias. In managing people with low-grade lymphomas, treatment may include these options according to the British Society of Haematology (2020) and ESMO guidelines general concepts:
If there is an indication that a patient’s cancer has returned, care should be provided under the guidance of a treating specialist. Each patient should be evaluated to determine if referral to the original multidisciplinary team is necessary. Often referral back to the original multidisciplinary team will not be necessary unless there are obvious aspects of care involving different therapeutic and supportive care disciplines not otherwise accessible. The multidisciplinary team may include new members such as palliative care specialists.
Treatment will depend on the location, extent of recurrent or residual disease, previous management and the patient’s preferences. In managing people with a low-grade lymphoma, treatment may include these options: Follicular and marginal zone lymphomas (ESMO 2020) Mantle cell lymphoma
Advance care planning is important for all patients with a cancer diagnosis but especially those with relapsed disease. Patients should be encouraged to think and talk about their healthcare values and preferences with family or carers, appoint a substitute decision-maker and consider developing an advance care directive to convey their preferences for future health care in the event they become unable to communicate their wishes (Australian Government Department of Health 2021a). More information Refer to section 4.3 ‘More information’ for links to resources. Refer patients and carers to Advance Care Planning Australia or to the Advance Care Planning National Phone Advisory Service on 1300 208 582.
Early referral to palliative care can improve the quality of life for people with cancer and in some cases may be associated with survival benefits (Haines 2011; Temel et al. 2010; Zimmermann et al. 2014). The treatment team should emphasise the value of palliative care in improving symptom management and quality of life to patients and their carers. Refer to section 4.3 for more detailed information. The lead clinician should ensure timely and appropriate referral to palliative care services. Referral to palliative care services should be based on the patient’s need and potential for benefit, not prognosis. More information Refer to the end of section 4.3 ‘Palliative care’ for links to resources.
Novel therapies are substantially improving the overall survival and quality of life for patients with low-grade lymphomas. The treatment team should be aware of and support the patient to take part in research and clinical trials where available and appropriate. For more information visit:
See validated screening tools mentioned in Principle 4 ‘Supportive care’. A number of specific challenges and needs may arise at this time for patients: Rehabilitation may be required at any point of the care pathway, from preparing for treatment through to palliative care. Issues that may need to be dealt with include managing cancer-related fatigue, improving physical endurance, achieving independence in daily tasks, returning to work and ongoing adjustment to cancer and its consequences. Exercise is a safe and effective intervention that improves the physical and emotional health and wellbeing of cancer patients. Exercise should be embedded as part of standard practice in cancer care and be viewed as an adjunct therapy that helps counteract the adverse effects of cancer and its treatment. The lead clinician should ensure there is adequate discussion with patients and carers about the diagnosis and recommended treatment, including treatment intent and possible outcomes, likely adverse effects and the supportive care options available. More information Refer to Principle 6 ‘Communication’ for communication skills training programs and resources.
Step 7 is concerned with maintaining the patient’s quality of life and meeting their health and supportive care needs as they approach the end of life, as well as the needs of their family and carers.
Some patients with advanced cancer will reach a time when active treatment is no longer appropriate. The team needs to share the principles of a palliative approach to care when making decisions with the patient and their family or carer. End-of-life care is appropriate when the patient’s symptoms are increasing and functional status is declining.
If the treatment team does not include a palliative care member, the lead clinician should consider referring the patient to palliative care services, with the general practitioner’s engagement. This may include inpatient palliative unit access (as required). The multidisciplinary team may consider seeking additional expertise from these professionals: The team might also recommend that patients access these services: If the patient does not already have an advance care directive in place, a designated member of the treatment team should encourage them to develop one in collaboration with their family or carer (Australian Government Department of Health 2021a). It is essential for the treatment team to consider the appropriate place of care, the patient’s preferred place of death and the support needed for the patient, their family and carers. The treatment team should also ensure that carers and families receive the information, support and guidance about their role according to their needs and wishes (Palliative Care Australia 2018). More information The treatment team can refer patients and carers to these resources:
Clinical trials may help improve palliative care and in managing a patient’s symptoms of advanced cancer (Cancer Council Victoria 2019). The treatment team should support the patient to participate in research and clinical trials where available and appropriate. For more information visit:
See validated screening tools mentioned in Principle 4 ‘Supportive care’. A number of specific challenges and needs may arise for patients at this time: These services and resources can help: For more information on supportive care and needs that may arise for different population groups, see Appendices A, B and C. The lead clinician is responsible for: The lead clinician should discuss end-of-life care planning to ensure the patient’s needs and goals are met in the appropriate environment. The patient’s general practitioner should be kept fully informed and involved in major developments in the patient’s illness path. For support with communication skills and training programs, see these sources:
The burden of cancer is not evenly spread across Australia. People experiencing socioeconomic disadvantage, Aboriginal and Torres Strait Islander communities, culturally diverse communities, people living with a disability, people with chronic mental health or psychiatric concerns and those who live in regional and rural areas of Australia have poorer cancer outcomes.
Cancer is the third leading cause of burden of disease for Aboriginal and Torres Strait Islander people. While Australia’s cancer survival rates are among the best in the world, Aboriginal and Torres Strait Islander people continue to experience a different pattern of cancer incidence and significant disparities in cancer outcomes compared with non-Indigenous Australians.
For Aboriginal and Torres Strait Islander people, health and connection to land, culture, community and identity are intrinsically linked. Health encompasses a whole-of-life view and includes a cyclical concept of life–death–life.
The distinct epidemiology of cancer among Aboriginal and Torres Strait Islander people, and unique connection to culture, highlight the need for a specific optimal care pathway for Aboriginal and Torres Strait Islander people with cancer. Ensuring this pathway is culturally safe and supportive is vital to tackling the disparities for Aboriginal and Torres Strait Islander people.
Published in 2018, the Optimal care pathway for Aboriginal and Torres Strait Islander people with cancer provides guidance to health practitioners and service planners on optimal care for Aboriginal and Torres Strait Islander people with cancer across the cancer continuum.
In addition to the key principles underpinning tumour-specific pathways, these are the key concepts that are fundamental to Aboriginal and Torres Strait Islander health:
- providing a holistic approach to health and wellbeing
- providing a culturally appropriate and culturally safe service
- acknowledging the diversity of Aboriginal and Torres Strait Islander peoples
- understanding the social determinants and cultural determinants of health (Cancer Australia 2015).
To view the Optimal care pathway for Aboriginal and Torres Strait Islander people with cancer, visit the Cancer Australia website . To view the consumer resources – Checking for cancer and Cancer, visit the Cancer Australia website
For people from culturally diverse backgrounds in Australia, a cancer diagnosis can come with additional complexities, particularly when English proficiency is poor. In many languages there is not a direct translation of the word ‘cancer’, which can make communicating vital information difficult. Perceptions of cancer and related issues can differ greatly in people from culturally
diverse backgrounds and this can affect their understanding and decision making after a cancer diagnosis. In addition to different cultural beliefs, when English language is limited there is potential for miscommunication of important information and advice, which can lead to increased stress and anxiety for patients.
A professionally trained interpreter (not a family member or friend) should be made available when communicating with people with limited English proficiency. Navigation of the Australian healthcare system can pose problems for those with a non-Anglo culture, and members of the treatment teams should pay particular attention to supporting these patients.
The Australian Cancer Survivorship Centre has developed a glossary of more than 700 cancer terms in nine different languages. The multilingual glossary has been designed as a resource for professional translators, interpreters and bilingual health professionals working in the cancer
field. The glossary is a unique tool that enables language professionals with access to accurate, consistent and culturally appropriate terminology.
Visit the Peter Mac website to see the glossary.
Disability, which can be physical, intellectual or psychological, may have existed before the cancer diagnosis or may be new in onset (occurring due to the cancer treatment or incidentally). Adjusting to life with a disability adds another challenge to cancer care and survivorship.
Several barriers prevent people with disabilities from accessing timely and effective health care (AIHW 2017):
- physical limitations
- competing health needs
- the trauma of undergoing invasive procedures
- potential barriers associated with obtaining informed consent
- failure to provide assistance with communication
- lack of information
- discriminatory attitudes among healthcare
In caring for people with disabilities and a cancer diagnosis, the Australian Institute of Health and Welfare disability flag should be used at the point of admittance to correctly identify and meet the additional requirements of a person with disability. Facilities should actively consider access requirements, and health practitioners should make reasonable adjustments where required.
Patients aged between seven and 65 years who have a permanent or significant disability may be eligible for support or funding through the National Disability Insurance Scheme (National Disability Insurance Agency 2018). More information can be found on the NDIS website. Patients aged 65 years or older (50 years or older for Aboriginal or Torres Strait Islander people) may be eligible for subsidised support and services through aged care services. An application to determine eligibility can be completed online over the phone. More information can be found at the My Aged Care website .
More information
‘Talking End of Life’ is a resource that shows how to teach people with intellectual disability about end of life. It is designed for disability support workers but is also helpful for others including families, health professionals and educators.
To view the resource, visit the Talking End of Life website <www.caresearch.com.au/tel/tabid/4881/Default.aspx>.
Planning and delivering appropriate cancer care for older people can present a number of challenges. This could also be true for frail people or those experiencing comorbidities. Effective communication between oncology and geriatrics departments will help facilitate best practice care, which takes into account physiological age, complex comorbidities, risk of adverse events and drug interactions, as well as the implications of cognitive impairment on suitability of treatment and consent (Steer et al. 2009).
At a national interdisciplinary workshop convened by the Clinical Oncology Society of Australia,
it was recommended that people over the age of 70 undergo some form of geriatric assessment, in line with international guidelines (COSA 2013; palliAGED 2018). Screening tools can be used to identify those patients in need of a comprehensive geriatric assessment (Decoster et al. 2015).
This assessment can be used to help determine life expectancy and treatment tolerance and guide appropriate referral for multidisciplinary intervention that may improve outcomes (Wildiers et al. 2014).
Frailty is not captured through traditional measures of performance status (e.g. ECOG) and includes assessment in the domains of:
- function
- comorbidity
- presence of geriatric syndromes
- nutrition
- polypharmacy
- cognition
- emotional status
- social
In recent years, adolescent and young adult oncology has emerged as a distinct field due to lack of progress in survival and quality-of-life outcomes.
The significant developmental change that occurs during this life stage complicates a diagnosis of cancer, often leading to unique physical, social and emotional effects for young people at the time of diagnosis and throughout the cancer journey (Smith et al. 2012).
In caring for young people with cancer, akin to the comorbidities that require specific care in the older cancer population, the treatment team needs to pay careful attention to promoting normal development (COSA 2014). This requires personalised assessments and management involving a multidisciplinary, disease-specific, developmentally targeted approach that adheres to the following principles:
- understanding the developmental stages of adolescence and supporting normal adolescent health and development alongside cancer management
- understanding and supporting the rights of young people
- communication skills and information delivery that are appropriate to the young person
- meeting the needs of all involved, including the young person, their carers and their family
- working with educational institutions and workplaces
- considering survivorship and palliative care
An oncology team caring for an adolescent or young adult with cancer should be able to demonstrate these specific areas of expertise:
- be able to ensure access to expert adolescent and young adult health providers who have knowledge specific to the biomedical and psychosocial needs of the population
- understand the biology and current management of the disease in the adolescent and young adult age group
- consider participating in research and clinical trials for each patient
- engage in proactive discussion and management of fertility preservation, late effects of treatment, ongoing need for contraception, and psychosocial and psychosexual needs
- provide treatment in an environment that is friendly to adolescents and young
In general, people from lower socioeconomic groups are at greater risk of poor health, have higher rates of illness, disability and death, and live shorter lives than those from higher socioeconomic groups (AIHW 2016). People experiencing socioeconomic disadvantage are less likely to participate in screening programs, more likely to be obese, less likely to exercise and much more likely to smoke, which are all risk factors for cancer. In 2010–2014 age-standardised cancer incidence rates were higher in the lowest socioeconomic areas compared with the highest socioeconomic areas for all cancers combined (Cancer Australia 2019b).
Socioeconomic status and low health literacy are closely correlated. Therefore, effective communication with patients and carers is particularly important given the prevalence of low health literacy in Australia (estimated at 60 per cent of Australian adults) (ACSQHC 2014).
Consideration should be taken for cancer patients experiencing socioeconomic disadvantage to reduce their risk of being underserved for health care.
A diagnosis of cancer may present additional challenges to people who have pre-existing chronic mental health or psychiatric concerns, resulting in exacerbation of their mental health symptoms. This may include heightened anxiety, worsening depression or thoughts of self-harm.
As poor adjustment and coping can affect treatment decisions, people who are known to have a mental health diagnosis need psychosocial assessment in the oncology setting to formulate a plan for ongoing support throughout treatment.
Psychosocial support can assist with challenges in communicating with health professionals, enhance understanding of the treatment journey, ensure capacity for consent to treatment options and improve compliance with treatment requests. A referral for psychosocial support from a health professional to the psycho-oncology team can ensure these patients are provided with targeted interventions or referrals to community-based services that may mitigate problems associated with the impacts of social isolation that frequently accompany chronic mental ill-health.
Many patients with chronic mental health problems may be well known to external service providers. Psycho-oncology health professionals can form meaningful partnerships with existing service providers to optimise patient care throughout treatment and beyond.
Drug use disorders fall within the area of mental health conditions. People who are opiate dependent may have specific and individual requirements regarding pain management and their own preference for type of opiate prescribed or used.
People who identify as sexually or gender diverse may have unique needs following a cancer diagnosis. Sexually or gender diverse identities include (but are not limited to) people who identify as lesbian, gay, bisexual or transgender. There is no universally agreed upon initialism to describe this community, with other terms such as queer/questioning (Q), intersex (I), asexual (A) and pansexual
(P) often included, as well as a plus symbol (+) indicating inclusivity of other identities not explicitly mentioned. For the purposes of this document, this community is referred to as LGBTQI+.
Sexual orientation and gender identity are relevant across the entire spectrum of cancer care, from prevention to survivorship and end-of-life care. LGBTQI+ people are less likely to participate in cancer screening, and some segments of the LGBTQI+ community exhibit elevated rates of specific cancer risk factors – for example, higher rates of smoking and alcohol use. Regarding treatment, there may be unique factors relevant to LGBTQI+ people that may affect decision making. Additionally, the LGBTQI+ population experiences higher rates of anxiety, depression and
stressful life circumstances, and may be at risk of inferior psychosocial outcomes following a cancer diagnosis. LGBTQI+ people are also more likely to be estranged from their families of origin, and for older people, less likely to have adult children who may provide support and care.
Barriers to care for LGBTQI+ people include past negative interactions with healthcare systems, experiences or fear of discrimination and harassment in healthcare settings, assumptions of cisgender/heterosexual identity, lack of recognition or exclusion of same-sex partners from care, and a lack of relevant supportive care and information resources.
To provide safe and appropriate care for LGBTQI+ people with cancer, healthcare providers should:
- display environmental cues to show an inclusive and safe setting for LGBTQI+ patients
- avoid assumptions about the sexual orientation or gender identity of patients and their partners
- facilitate positive disclosure of sexual orientation or gender identity
- include same-sex/gender partners and families of choice in care
- be aware of relevant supportive care and information resources
- provide non-judgemental, patient-centred
Supportive care in cancer refers to the following five domains:
- the physical domain, which includes a wide range of physical symptoms that may be acute, relatively short lived or ongoing, requiring continuing interventions or rehabilitation
- the psychological domain, which includes a range of issues related to the patient’s mental health wellbeing and personal relationships
- the social domain, which includes a range of social and practical issues that will affect the patient, carer and family such as the need for emotional support, maintaining social networks and financial concerns
- the information domain, which includes access to information about cancer and its treatment, recovery and survivorship support services and the health system overall
- the spiritual domain, which focuses on the patient’s changing sense of self and challenges to their underlying beliefs and existential concerns (Palliative Care Victoria 2019).
Fitch’s (2000) model of supportive care recognises the variety and level of intervention required at each critical point as well as the need to be specific to the individual patient (Figure A1). The model targets the type and level of intervention required to meet patients’ supportive care needs.
Figure A1: Fitch’s tiered approach to supportive care

Consider a referral to a psychologist, psychiatrist, pastoral/spiritual care practitioner, social worker, specialist nurse or a relevant community-based program. For patients with low-grade lymphomas, referral to one or more of these services should be strongly considered at diagnosis (including for patients embarking on a ‘watch and wait’ approach), when starting treatment, with any subsequent treatments and for post-treatment survivorship support.
The following is a general checklist for initiation of referral, noting that due to the long trajectory of survival with low-grade lymphomas, early referral may put in place tools for patients to develop positive coping strategies that are useful at many timepoints in their disease:
- displaying emotional cues such as tearfulness, distress that requires specialist intervention, avoidance or withdrawal
- being preoccupied with or dwelling on thoughts about cancer and death
- displaying fears about the treatment process or the changed goals of their treatment
- displaying excessive fears about cancer progression or recurrence
- worrying about loss associated with their daily function, dependence on others and loss of dignity
- becoming isolated from family and friends and withdrawing from company and activities that they previously enjoyed
- feeling hopeless and helpless about the effect that cancer is having on their life and the disruption to their life plans
- struggling to communicate with family and loved ones about the implications of their cancer diagnosis and treatment
- experiencing changes in sexual intimacy, libido and function
- struggling with the diagnosis of recurrent disease
- having difficulties quitting smoking (refer to Quitline on 13 7848) or with other drug and alcohol use
- having difficulties transitioning to palliative
Additional considerations that may arise for the multidisciplinary team include:
- support for the carer – encourage referrals to psychosocial support from a social worker, psychologist or general practitioner
- referral to an exercise physiologist or physiotherapist as a therapeutic approach to prevent and manage psychological health
- referral to wellness-after-cancer programs to provide support, information and offer
Complementary therapies may be used together with conventional medical treatments to support and enhance quality of life and wellbeing. They do not aim to cure the patient’s cancer. Instead, they are used to help control symptoms such as pain and fatigue (Cancer Council Australia 2019).
The lead clinician or health professional involved in the patient’s care should discuss the patient’s use (or intended use) of complementary therapies not prescribed by the multidisciplinary team to assess safety and efficacy and to identify any potential toxicity or drug interactions.
The lead clinician should seek a comprehensive list of all complementary and alternative medicines being taken and explore the patient’s reason for using these therapies and the evidence base.
A transparent and honest discussion that is free from judgement should be encouraged.
While some complementary therapies are supported by strong evidence, others are not. For such therapies, the lead clinician should discuss their potential benefits and use them alongside conventional therapies (NHMRC 2014).
If the patient expresses an interest in using complementary therapies, the lead clinician should consider referring patients to health providers within the multidisciplinary team who have expertise in the field of complementary and alternative therapies (e.g. a clinical pharmacist, dietitian or psychologist) to assist them to reach an informed decision. Costs of such approaches should
be part of the discussion with the patient and considered in the context of evidence of benefit.
The lead clinician should assure patients who use complementary therapies that they can still access a multidisciplinary team review and encourage full disclosure about therapies being used.
More information
- See Cancer Australia’s position statement on complementary and alternative therapies
- See the Clinical Oncological Society of Australia’s position statement Use of complementary and alternative medicine by cancer patients
Advance Care Planning Australia
Advance Care Planning Australia provides national advance care planning resources for individuals, families, health professional and service providers. Resources include a national advisory service, information resources, a legal forms hub and education modules.
- Telephone: 1300 208 582
- Website
Australian Cancer Survivorship Centre
The Australian Cancer Survivorship Centre has developed information resources and events to help people move from initial treatment to post treatment and beyond, including those receiving maintenance treatments. While they do not provide clinical advice, they connect with a range of providers to enable improved care.
- Telephone: (03) 8559 6220
- Website
Australian Commission on Safety and Quality in Health Care
The Australian Commission on Safety and Quality in Health Care has developed a resource for patients and carers explaining the coordination of care that patients should receive from their health service during cancer treatment. The resource is called What to expect when receiving medication for cancer care.
Beyond Blue
Beyond Blue provides information about depression, anxiety and related disorders, as well as about available treatment and support services.
- Telephone: 1300 22 4636
- Website
Cancer Australia
Cancer Australia provides information for consumers, carers and their families including printed resources and video content.
Cancer Council’s Cancer Information and Support Service
Cancer Council 13 11 20 is a confidential telephone support service available to anyone affected by cancer. This service acts as a gateway to evidence-based documented, practical and emotional support available through Cancer Council services and other community organisations. Calls will be answered by a nurse or other oncology professional who can provide information relevant to a patient’s or carer’s situation. Health professionals can also access this service.
- Telephone: 13 11 20 – Monday to Friday, 9.00am to 5.00pm (some states have extended hours)
- Website
Cancer Council’s Cancer Connect
Cancer Connect is a free and confidential telephone peer support service that connects someone who has cancer with a specially trained volunteer who has had a similar cancer experience.
A Connect volunteer can listen with understanding and share their experiences and ways of coping. They can provide practical information, emotional support and hope. Many people newly diagnosed with cancer find this one-to-one support very beneficial.
For more information on Cancer Connect call Cancer Council on 13 11 20.
Canteen
Canteen helps adolescents, young adults and parents to cope with cancer in their family. Canteen offers individual support services, peer support services and a youth cancer service, as well as books, resources and useful links.
- Telephone: 1800 835 932 to talk to a health professional about information and support for young people or 1800 226 833 for other enquiries
- Website
Clinical trial information
For a collection of clinical trials available in Australia see the following sources of information:
- Cancer Australia
- Australian New Zealand Clinical Trials Registry
- Australasian Leukaemia and Lymphoma Group
- ClinTrial Refer
- Clinical Trials for an international view.
CanEAT pathway
A guide to optimal cancer nutrition for people with cancer, carers and health professionals.
Guides to best cancer care
The short guides help patients, carers and families understand the optimal cancer care that should be provided at each step. They include optimal timeframes within which tests or procedures should be completed, prompt lists to support patients to understand what might happen at each step of their cancer journey and to consider what questions to ask, and provide information to help patients and carers communicate with health professionals.
The guides are located on an interactive web portal, with downloadable PDFs available in multiple languages.
Look Good, Feel Better
A free national community service program, run by the Cancer Patients Foundation, dedicated to teaching cancer patients how to manage the appearance-related side effects caused by treatment for any type of cancer.
- Telephone: 1800 650 960
- Website
Leukaemia Foundation
The Leukaemia Foundation provides specialist support, funds leading-edge research and advocates for Australians diagnosed with blood cancer. The foundation guides patients and their loved ones through the emotional, physical and psychosocial challenges of a blood cancer diagnosis, treatment and survivorship.
The foundation’s team of qualified health professionals can answer questions, talk through concerns and connect patients to blood cancer support groups. The team can also help with practical concerns such as accommodation close to treatment, transport to appointments and financial assistance.
- Telephone: 1800 620 420
- Website
Lymphoma Australia
Lymphoma Australia helps patients and their families to understand their diagnosis and treatment options. Lymphoma Australia is the only incorporated charity in Australia dedicated to solely providing education,
support, awareness and advocacy initiatives for Australians touched by lymphoma and chronic lymphocytic leukaemia.
Lymphoma Australia provides information packs to patients and hospitals and host education days and webinars to help people better understand lymphoma. Its lymphoma specialist nurses deliver an essential service to patients and cancer nurses. Lymphoma Australia nurses can help navigate the lymphoma journey and connect patients with others and the appropriate support networks.
Quitline
Quitline is a confidential, evidence-based telephone counselling service. Highly trained Quitline counsellors use behaviour change techniques and motivational interviewing over multiple calls to help people plan, make and sustain a quit attempt.
Quitline is a culturally inclusive service for all, and Aboriginal counsellors are also available. Health professionals can refer patients to Quitline online or via fax.
- Telephone: 13 7848
- Website or the relevant website in your state or territory.
Australian Cancer Survivorship Centre
The Australian Cancer Survivorship Centre provides expertise in survivorship care, information, support and education. Its purpose is to support and enable optimal survivorship care.
- Telephone: (03) 8559 6220
- Website
Australian Commission on Safety and Quality in Health Care
The Australian Commission on Safety and Quality in Health Care has developed a guide for clinicians containing evidence-based strategies to support clinicians to understand and fulfil their responsibilities to cancer patients.
This guide is particularly relevant to Steps 3 to 6 of the optimal care pathway. The guide is titled NSQHS Standards user guide for medication management in cancer care for clinicians
Cancer Australia
Information for health providers including guidelines, cancer learnings, cancer guides, reports, resources, videos, posters and pamphlets.
Cancer Council Australia
Information on prevention, research, treatment and support provided by Australia’s peak independent cancer authority.
CanEAT pathway
A guide to optimal cancer nutrition for people with cancer, carers and health professionals.
eviQ
A clinical information resource providing health professionals with current evidence-based, peer-maintained, best practice cancer treatment protocols and information relevant to the Australian clinical environment.
National Aboriginal Community Controlled Health Organisation
The National Aboriginal Community Controlled Health Organisation (NACCHO) is the national leadership body for Aboriginal and Torres Strait Islander health in Australia. NACCHO provides advice and guidance to the Australian
Government on policy and budget matters and advocates for community-developed solutions that contribute to the quality of life and improved health outcomes for Aboriginal and Torres Strait Islander people.
National Health and Medical Research Council
Information on clinical practice guidelines, cancer prevention and treatment.
advance care directive – voluntary person-led document that focus on an individual’s values and preferences for future health and medical treatment decisions, preferred outcomes and care. They are completed and signed by a competent person. They are recognised by specific legislation (statutory) or common law (non-statutory). Advance care directives can also appoint the substitute decision-maker(s) who can make decisions about health or personal care on the individual’s behalf if they are no longer able to make decisions themselves.
Advance care directives focus on the future health care of a person, not on the management of his or her assets. They come into effect when an individual loses decision-making capacity.
advance care planning – the process of planning for future health and personal care, where the person’s values, beliefs and preferences are made known so they can guide decision making at a future time when that person cannot make or communicate their decisions.
alternative therapies – treatments used in place of conventional medical treatment.
care coordinator – the health provider nominated by the multidisciplinary team to coordinate patient care. The care coordinator may change over time depending on the patient’s stage in the care pathway and the location and care in which care is being delivered.
complementary therapies – supportive treatment used in conjunction with conventional medical treatment. These treatments may improve wellbeing and quality of life and help people deal with the side effects of cancer.
end-of-life care – includes physical, spiritual and psychosocial assessment, and care and treatment, delivered by health professionals and ancillary staff. It also includes support of families and carers and care of the patient’s body after their death.
immunotherapy – a type of cancer treatment that helps the body’s immune system to fight cancer. Immunotherapy can boost the immune system to work better against cancer or remove barriers to the immune system attacking the cancer.
indicator – a documentable or measurable piece of information regarding a recommendation in the optimal care pathway.
informed financial consent – the provision of cost information to patients, including notification of likely out-of-pocket expenses (gaps), by all relevant service providers, preferably in writing, before admission to hospital or treatment (Australian Government Department of Health 2017).
lead clinician – the clinician who is nominated as being responsible for individual patient care. The lead clinician may change over time depending on the stage of the care pathway and where care is being provided.
minimal residual disease (MRD) – a small number of cancer cells left in the body after treatment
multidisciplinary care – an integrated team approach to health care in which medical and allied health providers consider all relevant treatment options and collaboratively develop an individual treatment plan for each patient.
multidisciplinary team – comprises the core disciplines that are integral to providing good care. The team is flexible in approach, reflects the patient’s clinical and psychosocial needs and has processes to facilitate good communication.
multidisciplinary team meeting – a meeting of health professionals from one or more clinical disciplines who together make decisions about recommended treatment of patients.
optimal care pathway – the key principles and practices required at each stage of the care pathway to guide the delivery of consistent, safe, high-quality and evidence-based care for all people affected by cancer.
performance status – an objective measure of how well a patient can carry out activities of daily life.
primary care health professional – in most cases this is a general practitioner but may also include general practice nurses, community nurses, nurse practitioners, allied health professionals, midwives, pharmacists, dentists and Aboriginal health workers.
prognostic assessment – evaluation of clinical features (e.g. pathological, biochemical, molecular, genetic, simple clinical measurements) to predict a patient’s likelihood of responding to treatment, developing disease or experiencing a medical event.
relative survival – the probability of being alive for a given amount of time after diagnosis compared with the general population.
risk stratification – a systematic process to target, identify an select patients who are at risk of poorer health outcomes, and who are expected to benefit most from a particular intervention or suite of interventions.
spiritual care – the aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred.
substitute decision-maker – a person permitted under the law to make decisions on behalf of someone who does not have competence or capacity.
supportive care – care and support that aims to improve the quality of life of people living with cancer, cancer survivors and their family and carers and particular forms of care that supplement clinical treatment modalities.
survivorship – an individual is considered a cancer survivor from the time of diagnosis, and throughout their life; the term includes individuals receiving initial or maintenance treatment, in recovery or in the post-treatment phase.
survivorship care plan – a formal, written document that provides details of a person’s cancer diagnosis and treatment, potential late and long-term effects arising from the cancer and its treatment, recommended follow-up, surveillance, and strategies to remain well.
targeted therapy – a medicine that blocks the growth and spread of cancer by interfering with specific molecules.
We acknowledge the Traditional Owners of Country throughout Australia and their continuing connection to the land, sea and community. We pay our respects to them and their cultures and to Elders past, present and emerging.
This work is available from the Leukaemia Foundation website and from the Cancer Council website.
This edition published in October 2021. ISBN: 978-0-6453299-5-7
Leukaemia Foundation and Australian Government Department of Health 2021, Optimal care pathway for people with low-grade lymphomas, 1st edn, Leukaemia Foundation of Australia.
Enquiries about this publication can be sent to bloodcancerpartnerships@leukaemia.org.au.
Our thanks to the following health professionals, consumer representatives, stakeholders and organisations consulted in developing this optimal care pathway.
Professor Judith Trotman (Co Chair), Haematologist, Concord Repatriation General Hospital, University of Sydney
Dr Nicole Wong Doo (Co Chair), Haematologist, Concord Repatriation and General Hospital, University of Sydney
Rebecca Beck, Lymphoma Care Nurse
Associate Professor Belinda A Campbell, Radiation Oncologist, Peter MacCallum Cancer Centre and University of Melbourne
Associate Professor Tara Cochrane, Haematologist, Gold Coast University Hospital, Southport, Queensland, Griffiths University Queensland
Serg Duchini, Consumer Representative, Chair, Lymphoma Australia
Associate Professor Kenneth Lee, Anatomical Pathologist, NSW Health Pathology, Concord Repatriation General Hospital, University of Sydney Medical School
Dr Robert Menz, General Practitioner, The Royal Australian College of General Practitioners
Sharon Millman, Chief Executive Officer, Lymphoma Australia
Dr Anthoulla Mohamudally, Palliative Care Physician, Royal Prince Alfred Hospital, Sydney
Professor Stephen Opat, Haematologist, Monash Health, Clinical Professor Monash University, Australasian Lymphoma and Related Disease Registry
Dr Emma Palfreyman, Haematologist, Royal Darwin Hospital
Kerry Wagland, Registered Psychologist, Headway Health, ICON Cancer Centre
Associate Professor Christina Brown, Haematologist, Royal Prince Alfred Hospital
Professor Chan Cheah, Haematologist, Sir Charles Gardiner Hospital, Pathwest,
Linear Clinical Research, Clinical Professor
of Haematology, University of Western Australia, Blood Cancer Research WA, Australasian Lymphoma Alliance
Clinical Associate Professor Anna Johnston, Haematologist, Royal Hobart Hospital, University of Tasmania
Dr Matthew Ku, Haematologist and Lymphoma Lead, St Vincent’s Hospital, University of Melbourne
Medical colleges, peak organisations and government representatives
Associate Professor Peter Mollee (Chair), Haematologist Princess Alexandra Hospital, Australasian Leukaemia and Lymphoma Group, Associate Professor, University of Queensland
Australian Capital Territory Health Allied Health Professions Australia
Australian and New Zealand Children’s Haematology/Oncology Group
Australia and New Zealand Transplant and Cellular Therapies
Australasian Association of Nuclear Medicine Specialists
Australasian College of Emergency Medicine Australasian Leukaemia & Lymphoma Group
Australian and New Zealand Society of Palliative Care
Australian College of Nursing
Australian College of Rural and Remote Medicine Australian Government Department of Health and Ageing Australian Medical Association
Beyond Blue Cancer Australia
Cancer Council of Australia Cancer Council Victoria Cancer Institute NSW
Cancer Nurses Society of Australia Canteen
Clinical Oncology Society of Australia
Haematology Society of Australia & New Zealand
Launceston General Hospital Leukaemia Foundation Lymphoma Australia
Medical Oncology Group of Australia Myeloma Australia
Northern Territory Department of Health Palliative Care Australia
Private Cancer Physicians of Australia Queensland Health
Rare Cancers Australia Redkite
Royal Australasian College of Physicians
Royal Australian and New Zealand College of Radiologists
Royal College of Pathologists of Australasia South Australia Health
Tasmanian Department of Health and Human Services
The Royal Australian College of General Practitioners
Victorian Department of Health
Western Australia Cancer and Palliative Care Network
Dr Caroline M Bateman, Paediatric Haematologist and Oncologist, Cancer Centre for Children, The Children’s Hospital at Westmead
Julia Brancato, Optimal Care Pathways Project Coordinator, Cancer Council Victoria
Dr Peter Diamond, Project Secretariat, Leukaemia Foundation
Associate Professor Michael Dickinson, Haematologist, Lymphoma Australia, Peter MacCallum Cancer Centre, Royal Melbourne Hospital, University of Melbourne
Associate Professor Anoop Enjeti, Haematologist, John Hunter Hospital, Senior Staff Haematologist, Calvary Mater Hospital, Conjoint Associate Professor, University of Newcastle
Emily Forrest, Project Secretariat, Leukaemia Foundation
Fiona Haigh, Project Secretariat, Leukaemia Foundation
Deborah Henderson, Consumer Representative
Professor Tim Hughes, Haematologist, South Australian Health and Medical Research Institute (SAHMRI), University of Adelaide, Royal Adelaide Hospital
Professor Steven Lane, Haematologist, Royal Brisbane and Women’s Hospital, QIMR
Berghofer Medical Research Institute, University of Queensland
Caroline Nehill, Director National Cancer Control, Cancer Australia
Professor H. Miles Prince AM, Haematologist, Epworth Healthcare and Haematologist
Peter MacCallum Cancer Centre
Professor Hang Quach, Haematologist, University of Melbourne, St. Vincent’s Hospital Melbourne
Catriona Rafael, Project Secretariat, Leukaemia Foundation
Professor Andrew Roberts AM, Haematologist and Bone Marrow Transplant Physician, Royal Melbourne Hospital, Peter MacCallum Cancer Centre, University of Melbourne, Walter and Eliza Hall Institute
Professor John Seymour AM, Haematologist, Peter MacCallum Cancer Centre, Royal Melbourne Hospital, University of Melbourne
Delaine Smith, Chief Executive Officer, Australasian Leukaemia and Lymphoma Group
Professor Judith Trotman, Haematologist, Concord Repatriation General Hospital, University of Sydney
Megan Varlow, Director Cancer Control Policy, Cancer Council Australia
Dr Nicole Wong Doo, Haematologist, Concord Repatriation and General Hospital, University of Sydney
Our thanks also to the Blood Cancer Taskforce, which recommended the development of optimal care pathways for all the major blood cancer subtypes as part of the National Strategic Action Plan for Blood Cancer (2020). The National Action Plan was commissioned by the Federal Government and developed by the Blood Cancer Taskforce, with support from the Leukaemia Foundation.
Not all patients with lgl require ongoing input from a multidisciplinary team. Where required, the multidisciplinary team may include the following members:
- care coordinator (as determined by multidisciplinary team members)*
- haematologist*
- infectious diseases physician*
- nurse (with appropriate expertise or under the supervision of nurses with appropriate expertise)*
- pathologist including pathologist with molecular genetic expertise*
- pharmacist*
- Aboriginal health practitioner, Indigenous liaison officer or remote general practitioner
- fertility specialist
- spiritual/pastoral care
- clinical trials coordinator
- dentist
- dietitian
- exercise physiologist
- general practitioner
- genetic counsellor
- geriatrician
- nuclear medicine physician
- occupational therapist
- palliative care specialist
- physiotherapist
- psychiatrist
- psychologist
- radiation oncologist
- radiologist/imaging specialists
- social worker
- spiritual/pastoral
* Denotes core members. Core members of the multidisciplinary team are expected to attend most multidisciplinary team meetings either in person or remotely.
Abar L, Sobiecki JG, Cariolou M, Nanu N, Vieira AR, Stevens C, et al. 2019 ‘Body size and obesity during adulthood, and risk of lympho- haematopoietic cancers: an update of the WCRF-AICR systematic review of published prospective studies’, Annuals of Oncology, vol.30, no.4, pp. 528-541.
Arden JB 2015, Chapter 2: Promoting brain health. In: Brain2Brain: enacting client change through the persuasive power of neuroscience, John Wiley & Sons, pp. 31–61.
Ardeshna KM, Smith P, Norton A, Hancock BW, Hoskin PJ, MacLennan KA, et al. 2003, ‘Long- term effect of a watch and wait policy versus immediate systemic treatment for asymptomatic advanced-stage non-Hodgkin lymphoma: a randomised controlled trial’, Lancet, vol. 362, no. 9383, pp. 516–522.
Armitage JO, Gascoyne RD, Lunning MA, Cavalli F 2017, ‘Non-Hodgkin lymphoma’, Lancet, vol. 390, no. 10091, pp. 298–310.
Australian Adult Cancer Pain Management Guideline Working Party 2019, Australian adult cancer pain management guideline: ‘Cancer pain management in adults’, Cancer Council Australia, Sydney, viewed 6 June 2019,
<https://wiki.cancer.org.au/australiawiki/index.php?oldid=191646>.
Australian Cancer Survivorship Centre 2010, ‘Survivorship care planning’, viewed 27 November 2013,
<http://122.102.106.143/cancersurvivorship/Home>.
Australian Cancer Survivorship Centre 2019, Community support organisations’ cancer survivorship care consensus statement, viewed 10 February 2020,
<https://www.petermac.org/sites/default/files/media-uploads/NGO_ConsensusStatement.pdf>.
Australian Clinical Trials 2015, ‘Potential benefits and risks’, National Health and Medical Research Council, Department of Industry,
Innovation and Science, Australian Government, Canberra, viewed 24 July 2019,
<https://www.australianclinicaltrials.gov.au/why-be-part-clinical-trial/potential-benefits-and-potential-risks>.
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2014, Health literacy: taking action to improve safety and quality, ACSQHC, Sydney, viewed 18 February 2020,
<https://www.safetyandquality.gov.au/sites/default/files/migrated/Health-Literacy-Taking-action-to-improve-safety-and-quality.pdf>.
Australian Commission for Safety and Quality in Health Care (ACSQHC) 2015, Credentialing health practitioners and defining their scope of clinical practice: a guide for managers and practitioners, ACSQHC, Sydney, viewed 18 February 2020, <https://www.safetyandquality.gov.au/publications-and-resources/resource-library/credentialing-health-practitioners-and-defining-their-scope-clinical-practice-guide-managers-and-practitioners>.
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2017, National Safety and Quality Health Service Standards guide for hospitals, ACSQHC, Sydney, viewed 18 February 2020,
<https://www.safetyandquality.gov.au/wp-content/uploads/2017/12/National-Safety-and-Quality-Health-Service-Standards-Guide-for-Hospitals.pdf>.
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2019a, Person-centred care, ACSQHC, Sydney, viewed 15 May 2020,
<https://www.safetyandquality.gov.au/our-work/partnering-consumers/person-centred-care>.
Australian Commission on Safety and Quality in Health Care (ACSQHC) 2019b, Australian Hospital Patient Experience Question Set, ACSQHC, Sydney, viewed 25 March 2020,
<https://www.safetyandquality.gov.au/our-work/indicators-measurement-and-reporting/australian-hospital-patient-experience-question-set>.







