STEP 2: Presentation, initial investigations and referral
This step outlines the process for establishing a diagnosis and appropriate referral. The types of investigation undertaken by the general or primary practitioner depend on many factors including access to diagnostic tests, medical specialists and the woman’s preferences.
General practitioners play a crucial role in encouraging women to screen regularly.
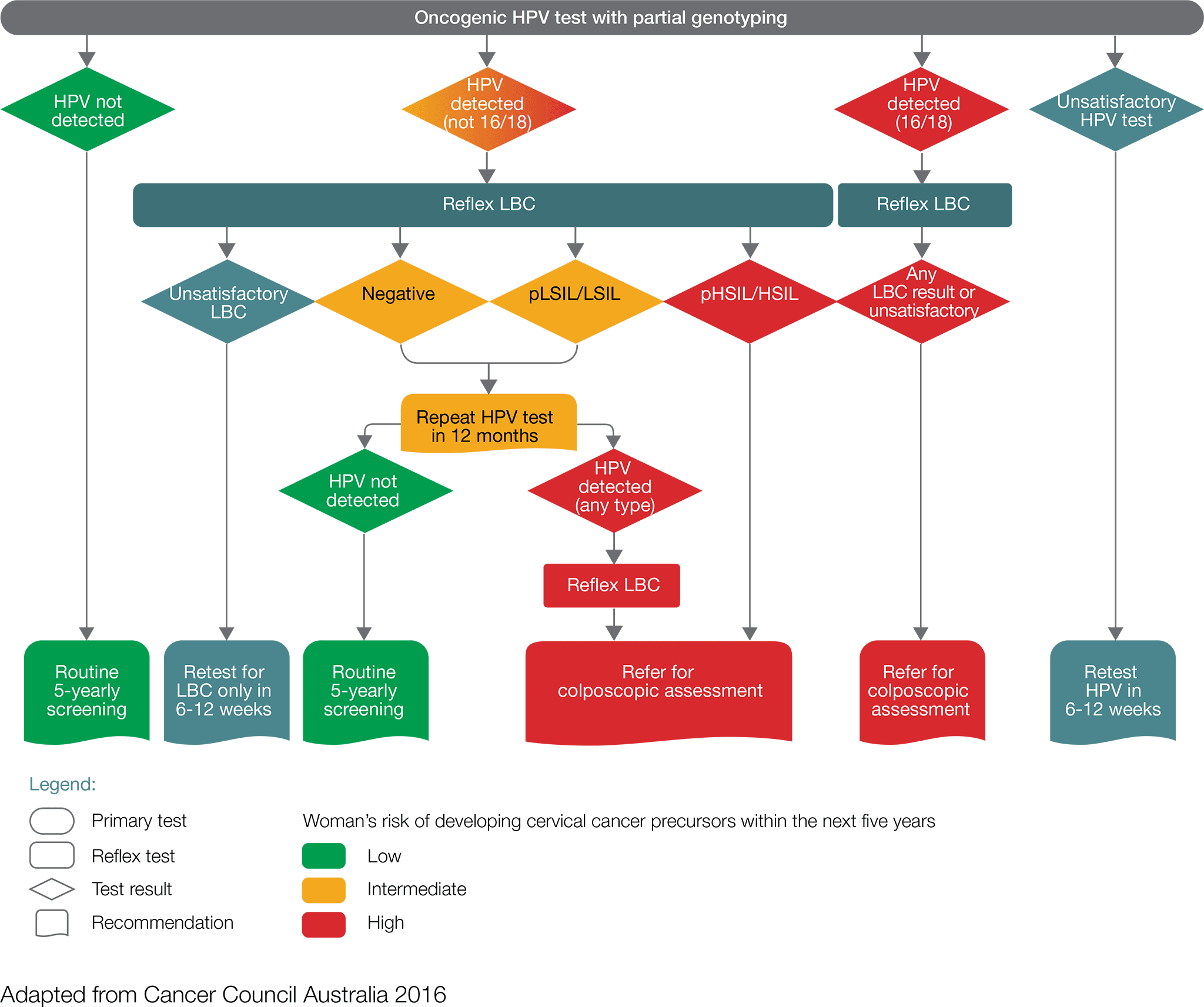
- Women with a positive oncogenic HPV (16/18) test result including those found through a self-collected sample should be referred directly for a colposcopic assessment, which will be informed by the result of reflex liquid-based cytology (LBC).
- Women with a positive oncogenic HPV (not 16/18) test result, with an LBC report of possible high-grade lesion or high-grade lesion should be referred directly for colposcopic assessment
- Women with a positive oncogenic HPV (not 16/18) test result, with an LBC report of negative or low-grade lesion, should have a repeat HPV test in 12 months.
- For women with a self-collected positive oncogenic HPV (not 16/18) they should be advised to visit their GP or healthcare professional to obtain a cervical sample for liquid-based cytology. If the liquid-based cytology result is possible high-grade or high-grade, the women should be referred for colposcopy ideally within 8 weeks.
At 12 months, repeat HPV testing:
- Women in whom oncogenic HPV is not detected should return to routine five-yearly clinician- collected screening.
- Women with a positive oncogenic HPV (any type) test result should be referred for a colposcopic assessment. If the repeat HPV test was self-collected, a cervical sample for LBC should be obtained at the time of the colposcopy.
While general practitioners recommendations will be informed by the results of the two tests (HPV test and LBC), a negative test should not preclude further investigations of signs and symptoms that suggest the presence of cervical cancer.
If a woman presents with symptoms at any age, whether or not she has been vaccinated against HPV, the symptoms should be investigated.
In the early stages of cervical cancer, there may be no symptoms at all. If symptoms occur, they commonly include:
- postcoital bleeding
- intermenstrual bleeding
- postmenopausal bleeding
- dyspareunia
- unusual or watery vaginal discharge.
Symptoms of advanced cervical cancer include:
- pelvic pain
- extreme fatigue
- kidney failure
- leg pain or swelling
- lower back pain.
At the time of specialist referral, an assessment informed by signs and symptoms, including a physical examination, co-test (simultaneous HPV and LBC tests), and blood tests (FBE) should occur. If the cervix appears abnormal (suspicious for cancer) on physical examination consider direct referral to a specialist gynaecological oncologist who is part of a multidisciplinary team. Where there is not an obvious cancer the flowchart should guide management.

If the diagnosis is suspected or confirmed with initial tests, then referral to a certified gynaecological oncologist who is a member of a multidisciplinary team is optimal.
Referral should include relevant past history, current history, family history, examination, investigations, psychosocial issues and current medications.
Timeframes should be informed by evidence-based guidelines (where they exist) while recognising that shorter timelines for appropriate consultations and treatment can reduce the woman’s distress.
The following recommended timeframes are based on expert advice from the Cervical Cancer Working Group(1):
- Cervical testing results should be available and the woman reviewed by her general practitioner within 30 days.
- Women with a positive oncogenic HPV (any type) test result and LBC report of invasive cancer should have a specialist appointment with a gynaecological oncologist within two weeks of the suspected diagnosis.
- Women with a positive oncogenic HPV (16/18) test result and reflex LBC prediction of any abnormality should be referred for a colposcopic assessment within eight weeks.
- Women with a positive oncogenic HPV (not 16/18) test result, with a LBC prediction of pHSIL/HSIL or any glandular abnormality, should be referred for a colposcopic assessment within eight weeks.
- Women with a suspected diagnosis of cervical cancer (symptomatic, abnormal cervix) should have a specialist appointment with a gynaecological oncologist within two weeks of the suspected diagnosis.
The supportive and liaison role of the general practitioner and practice team in this process is critical.
1: The multidisciplinary experts group who participated in a clinical workshop to develop content for the cervical cancer optimal care pathway are listed in the acknowledgements list.
An individualised clinical assessment is required to meet the identified needs of the woman, her carer and family; referral should be as required.
In addition to common issues identified in the Appendix, specific needs that may arise at this time include:
- treatment for physical symptoms such as pain and fatigue
- help with the emotional distress of dealing with a potential cancer diagnosis, anxiety/depression (particularly about potential loss of fertility), interpersonal problems, stress and adjustment difficulties
- referral to a fertility service for counselling and evaluation of options
- guidance about financial and employment issues (such as loss of income, travel and accommodation requirements for rural women and caring arrangements for other family members)
- appropriate information for women from culturally and linguistically diverse backgrounds.
Effective communication is essential at every step of the care pathway. Effective communication with the woman and her carer is particularly important given the prevalence of low health literacy in Australia (estimated at 60 per cent of Australian adults) (ACSQHC 2013).
The general or primary medical practitioner who made the referral is responsible for the woman until care is passed to another practitioner.
The general or primary medical practitioner may play a number of roles in all stages of the cancer pathway including diagnosis, referral, treatment, coordination and continuity of care as well as providing information and support to the woman and her family.
The general or primary practitioner should:
- provide the woman with information that clearly describes who they are being referred to, the reason for referral and the expected timeframe for appointments
- support the woman while waiting for the specialist appointment.
Cancer Council nurses are available to act as a point of information and reassurance during the anxiety-provoking period of awaiting further diagnostic information. Contact 13 11 20 nationally to speak to a cancer nurse. Health professionals can also access this service.







