2.1 Assessments by the general or primary medical practitioner
General practitioners play a crucial role in encouraging women to screen regularly.
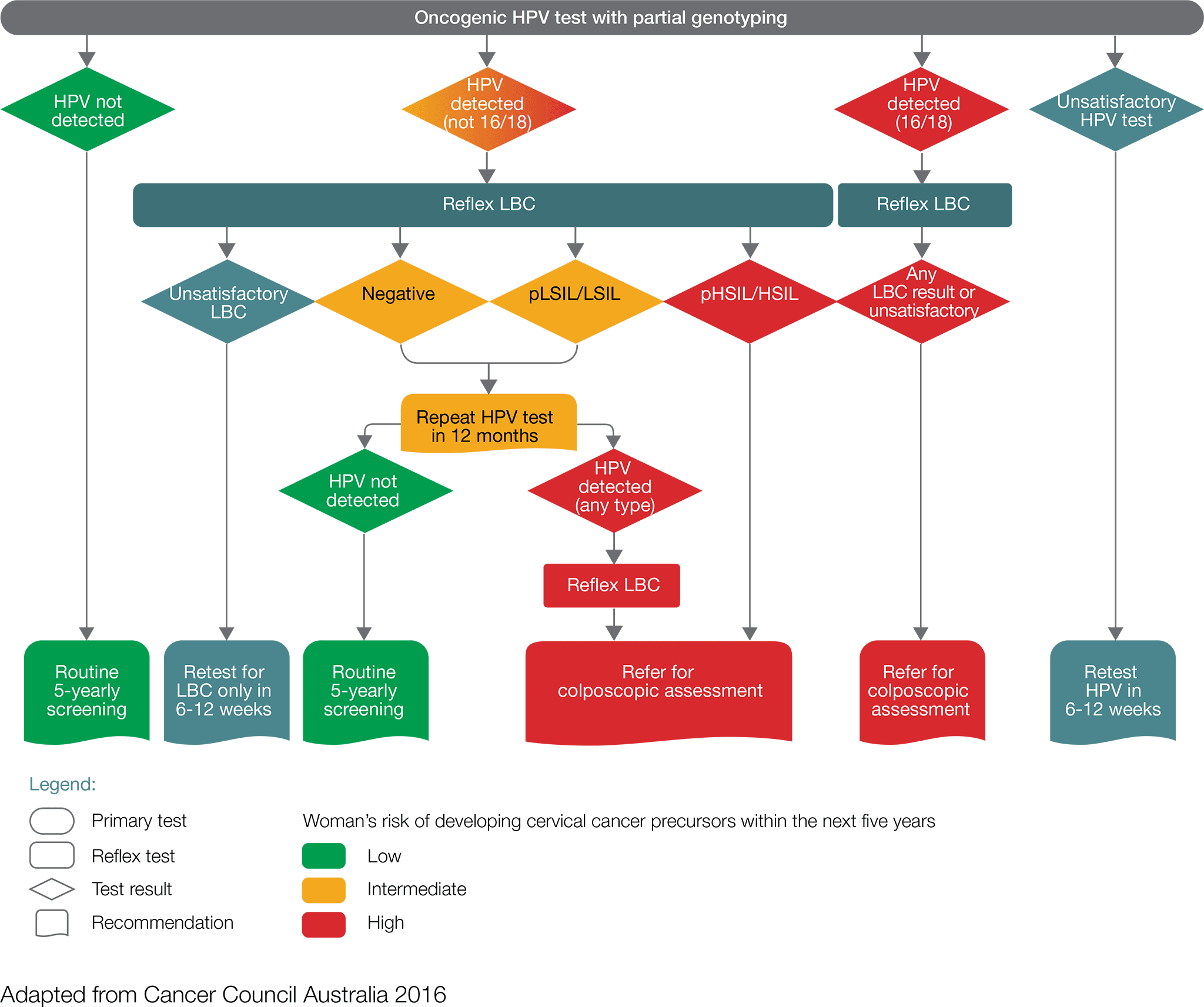
- Women with a positive oncogenic HPV (16/18) test result including those found through a self-collected sample should be referred directly for a colposcopic assessment, which will be informed by the result of reflex liquid-based cytology (LBC).
- Women with a positive oncogenic HPV (not 16/18) test result, with an LBC report of possible high-grade lesion or high-grade lesion should be referred directly for colposcopic assessment
- Women with a positive oncogenic HPV (not 16/18) test result, with an LBC report of negative or low-grade lesion, should have a repeat HPV test in 12 months.
- For women with a self-collected positive oncogenic HPV (not 16/18) they should be advised to visit their GP or healthcare professional to obtain a cervical sample for liquid-based cytology. If the liquid-based cytology result is possible high-grade or high-grade, the women should be referred for colposcopy ideally within 8 weeks.
At 12 months, repeat HPV testing:
- Women in whom oncogenic HPV is not detected should return to routine five-yearly clinician- collected screening.
- Women with a positive oncogenic HPV (any type) test result should be referred for a colposcopic assessment. If the repeat HPV test was self-collected, a cervical sample for LBC should be obtained at the time of the colposcopy.
While general practitioners recommendations will be informed by the results of the two tests (HPV test and LBC), a negative test should not preclude further investigations of signs and symptoms that suggest the presence of cervical cancer.
If a woman presents with symptoms at any age, whether or not she has been vaccinated against HPV, the symptoms should be investigated.
In the early stages of cervical cancer, there may be no symptoms at all. If symptoms occur, they commonly include:
- postcoital bleeding
- intermenstrual bleeding
- postmenopausal bleeding
- dyspareunia
- unusual or watery vaginal discharge.
Symptoms of advanced cervical cancer include:
- pelvic pain
- extreme fatigue
- kidney failure
- leg pain or swelling
- lower back pain.
At the time of specialist referral, an assessment informed by signs and symptoms, including a physical examination, co-test (simultaneous HPV and LBC tests), and blood tests (FBE) should occur. If the cervix appears abnormal (suspicious for cancer) on physical examination consider direct referral to a specialist gynaecological oncologist who is part of a multidisciplinary team. Where there is not an obvious cancer the flowchart should guide management.








